Histoplasma capsulatum: Difference between revisions
From IDWiki
Histoplasma capsulatum
Content deleted Content added
No edit summary |
|||
| (11 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
== |
==Background== |
||
===Microbiology=== |
|||
*Saprophytic environmental fungus withing the family Ascomycetes |
|||
* Dimorphic fungus; mold at room temperature, yeast at >37º C |
|||
*Thermally dimorphic, existing as a mold <35ºC and a yeast at >37ºC |
|||
** Mold: aerial hyphae with macroconidia |
|||
**Mold |
|||
*** Mold form is highly infectious, associated with lab-related outbreaks |
|||
***Mold form is highly infectious, associated with lab-related outbreaks |
|||
*** Mycelia have a typical appearance of spiked spherical conidia |
|||
***Septate hyaline mold with aerial hyphae with macroconidia, which are its identifying feature |
|||
** Yeast: |
|||
***Two types of conidia: tuberculate macroconidia (ovoid bodies 8 to 15 μm with spikes), and microconidia (small, smooth oval bodies 2 to 5 μm) |
|||
*** Non-infectious, once hanging out in your body |
|||
***Two colony types, brown (B) and albino (A) |
|||
*** Narrow-based budding |
|||
**Yeast |
|||
* ''H. capsulatum'' var. ''capsulatum'' most common worldwide, in various clades |
|||
***Non-infectious, once hanging out in your body |
|||
* ''H. capsulatum'' var. ''duboisii'' present in western Africa, has larger yeast forms |
|||
** |
***Small, 2 to 5 μm |
||
***Demonstrates multipolar narrow-based budding |
|||
***Does not look particularly different from other yeast, but may be intracellular |
|||
*Three variants |
|||
**''H. capsulatum'' var. ''capsulatum'', which is the most common worldwide, and is further divided into various clades |
|||
**''H. capsulatum'' var. ''duboisii'' which is only present in western Africa, and has larger yeast forms |
|||
***Can take up to 7 days to grow |
|||
**''H. capsulatum'' var. ''farciminosum'' |
|||
== |
===Epidemiology=== |
||
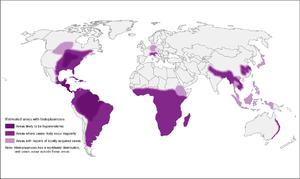
[[File:Histoplasmosis_map.png|thumb|Distribution of histoplasmosis]] |
|||
* |
*Endemic in many parts of the world |
||
** |
**Ohio and Mississippi River Valley systems (Central/Eastern US), where seroprevalence is as high as 80% in adults |
||
** |
**Probably up through St. Lawrence River as well |
||
** |
**Probably more broadly distributed, including Central and South America, South and East Asia, and Australia |
||
** |
**''H. capsulatum'' var. ''duboisii'' in western Africa |
||
* |
*Typically found in moist soil enriched with bat or bird droppings, which helps it to sporulate |
||
** |
**Disturbing the soil aerosolizes it, allowing the microconidia to be inhaled |
||
**Microconidia can be transported for miles by air currents |
|||
===Risk Factors=== |
|||
[[File:nihms680311f1.jpg|Histoplasmosis map from https://doi.org/10.1007/s40475-015-0044-0]] |
|||
*HIV, solid organ transplant, hematologic transplant |
|||
== Pathophysiology == |
|||
*Primary immunodeficiencies: X-linked hypogammaglobulinemia |
|||
===Pathophysiology=== |
|||
* Inhaled microconidia reach the alveolii and are phagocytosed by alveolar macrophages |
|||
** Innoculum size can be smaller with immunodeficiency |
|||
** Size of innoculation affects disease severity and progression |
|||
* Microconidia transform into budding yeasts, in a process that is dependent on macrophage calcium and iron |
|||
* They multiply inside macrophages, and translocate through the lymphatics |
|||
* Cellular immunity developed around 2 weeks later |
|||
** Response depends on IL-12 and TNF-alpha |
|||
** Organize to form granulomas to contain the infection |
|||
* Latent infection can reactivate, but rare |
|||
** Most common with infliximab |
|||
* In impaired cellular immunity, infection can become disseminated |
|||
*Inhaled microconidia reach the alveolii and are phagocytosed by alveolar macrophages |
|||
== Clinical Presentation == |
|||
**Innoculum size can be smaller with immunodeficiency |
|||
**Size of innoculation affects disease severity and progression |
|||
*Microconidia transform into budding yeasts, in a process that is dependent on intracellular macrophage calcium and iron |
|||
*They multiply inside macrophages, and translocate through the lymphatics |
|||
*Cellular immunity developed around 2 weeks later |
|||
**Response depends on IL-12 and TNF-α |
|||
**Organize to form granulomas to contain the infection |
|||
*Latent infection can reactivate, but rare |
|||
**Most common with [[infliximab]] |
|||
*In impaired cellular immunity, infection can become disseminated |
|||
==Clinical Manifestations== |
|||
* Often asymptomatic; in endemic areas, 50-80% of people skin-test positive or have radiographic evidence of previous infection |
|||
* Can cross tissue planes |
|||
*Spectrum of illness, related to the size of the inoculum, strain-specific virulence, and host immunity |
|||
=== Acute pulmonary histoplasmosis === |
|||
*Often asymptomatic; in endemic areas, 50-80% of people skin-test positive or have radiographic evidence of previous infection |
|||
*Can cross tissue planes |
|||
===Acute Pulmonary Histoplasmosis=== |
|||
* Fever, chill, malaise, headaches, myalgias, anorexia, cough, dyspnea, and chest pain |
|||
* Pneumonitis on chest x-ray, often with adenopathy |
|||
** "Buckshot" appearance? (Mandell) |
|||
* Can have rheumatologic sequelae in 5-10%, with arthralgias, arthritis, and erythema nodosum |
|||
* Can have pericarditis from the inflammatory response |
|||
* Hilar adenopathy can necrotize |
|||
* Usually self-limited, no need to treat unless longer than a month |
|||
*Fever, chill, malaise, headaches, myalgias, anorexia, cough, dyspnea, and chest pain |
|||
=== Progressive disseminated histoplasmosis === |
|||
**Spectrum from mild to severe |
|||
**Usually self-limited, no need to treat unless longer than a month |
|||
*Pneumonitis on chest x-ray, often with adenopathy |
|||
**"Buckshot" appearance? (Mandell) |
|||
*Can have rheumatologic sequelae in 5-10%, with arthralgias, arthritis, and erythema nodosum |
|||
*Can have pericarditis from the inflammatory response |
|||
*Hilar adenopathy can necrotize |
|||
===Progressive Disseminated Histoplasmosis=== |
|||
* Usually, though not exclusively, in immunocompromised pations |
|||
** Risk factors include CD4 <200, very old or very young, and therapeutic immunosuppression (pred, MMF, tac, MTX, TNF-alpha, other biologics |
|||
* Can be rapidly-progressing and acute, or more subacute |
|||
*Usually, though not exclusively, in immunocompromised patients |
|||
=== Acute progressive disseminated histoplasmosis === |
|||
**Risk factors include CD4 <200, very old or very young, and therapeutic immunosuppression ([[prednisone]], [[MMF]], [[tacrolimus]], [[methotrexate]], [[TNF-α inhibitors]], other biologics) |
|||
*Can be rapidly-progressing and acute, or more subacute |
|||
===Acute Progressive Disseminated Histoplasmosis=== |
|||
* Fever, weight loss, organomegaly, thrombocytopenia |
|||
* Meningitis or focal brain lesions |
|||
* Oral and GI mucosal ulcerations |
|||
* Adrenal insufficiency |
|||
*Fever, weight loss, organomegaly, thrombocytopenia |
|||
=== Chronic progressive disseminated histoplasmosis === |
|||
*Meningitis or focal brain lesions |
|||
*Oral and GI mucosal ulcerations |
|||
*Adrenal insufficiency |
|||
===Chronic Progressive Disseminated Histoplasmosis=== |
|||
* In normal hosts |
|||
* Absent or low-grade fever |
|||
* Longer course |
|||
* Most common finding is oropharyngeal lesion: deep, well-circumscribed, unrated, and painless |
|||
** Mimics squamous cell carcinoma |
|||
* Can also have hepatosplenomegaly, chronic meningitis, or chronic granulomatous hepatitis |
|||
*In normal hosts |
|||
=== Chronic cavitary histoplasmosis === |
|||
*Absent or low-grade fever |
|||
*Longer course |
|||
*Most common finding is oropharyngeal lesion: deep, well-circumscribed, unrated, and painless |
|||
**Mimics squamous cell carcinoma |
|||
*Can also have hepatosplenomegaly, chronic meningitis, or chronic granulomatous hepatitis |
|||
===Chronic Cavitary Histoplasmosis=== |
|||
* Typically seen in bullous emphysema |
|||
* Productive cough, dyspnea, low-grade fever, night sweats, weight loss |
|||
** Hemoptysis is rare |
|||
** Progressive without treatment |
|||
* Chest x-ray shows upper-lobe infiltrations, vacitation, and pleural thickening, similar to tuberculosis |
|||
*Typically seen in bullous emphysema |
|||
=== Fibrosing mediastinitis === |
|||
*Productive cough, dyspnea, low-grade fever, night sweats, weight loss |
|||
**Hemoptysis is rare |
|||
**Progressive without treatment |
|||
*Chest x-ray shows upper-lobe infiltrations, vacitation, and pleural thickening, similar to tuberculosis |
|||
===Fibrosing Mediastinitis=== |
|||
* Rare but serious |
|||
* Progressive fibrosis around hilar/mediatinal lymphadenopathy, wither unilateral or bilateral |
|||
* Can present with a SVC syndrome, obstruction of pulmonary vessels, or airway obstruction |
|||
* Can also present with recurrent pneumonias, hemoptysis, or respiratory failure |
|||
* 30% mortality |
|||
*Histoplasmosis is the most common cause of [[fibrosing mediastinitis]] |
|||
=== Other complications === |
|||
*Rare but serious |
|||
*Progressive fibrosis around hilar/mediastinal lymphadenopathy, wither unilateral or bilateral |
|||
**Occludes central vessels and airways |
|||
*Can present with a SVC syndrome, obstruction of pulmonary vessels, or airway obstruction |
|||
*Can also present with recurrent pneumonias, hemoptysis, or respiratory failure |
|||
*30% mortality |
|||
===Other Complications=== |
|||
* Ophthalmic uveitis |
|||
* Meningitis |
|||
* Endocarditis |
|||
*Ophthalmic posterior [[uveitis]] |
|||
== African histoplasmosis == |
|||
*Meningitis |
|||
*[[Infective endocarditis]] |
|||
===African Histoplasmosis=== |
|||
* ''H. capsulatum'' vars. ''capsulatum'' and ''duboisii'' coexist in Africa |
|||
* var. ''duboisii'' has more skin and skeletal manifestations |
|||
** Ulcers, nodules, or psoriaform lesions that can spontaneously resolve |
|||
*** Can cause a cold abscess, without inflammation |
|||
** Osteolytic bone lesions are common (50%) of cases |
|||
*** Skull and ribs most common |
|||
*** Can have sinus formation and cystic bone lesions |
|||
** May not have any evidence on CXR of prior pulmonary histoplasmosis |
|||
** Can also present with progressive disseminated disease, with fevers and multiorgan involvement |
|||
*** Combianation of granulomas and pus |
|||
*** Larger yeast is harder for macrophages to engulf |
|||
*''H. capsulatum'' vars. ''capsulatum'' and ''duboisii'' coexist in Africa |
|||
== Diagnosis == |
|||
*var. ''duboisii'' has more skin and skeletal manifestations |
|||
**Ulcers, nodules, or psoriaform lesions that can spontaneously resolve |
|||
***Can cause a cold abscess, without inflammation |
|||
**Osteolytic bone lesions are common (50%) of cases |
|||
***Skull and ribs most common |
|||
***Can have sinus formation and cystic bone lesions |
|||
**May not have any evidence on CXR of prior pulmonary histoplasmosis |
|||
**Can also present with progressive disseminated disease, with fevers and multiorgan involvement |
|||
***Combianation of granulomas and pus |
|||
***Larger yeast is harder for macrophages to engulf |
|||
==Diagnosis== |
|||
* Fungal culture of sputum (chronic cavitary), or blood or bone marrow aspirate (disseminated), or CSF (CNS histo) |
|||
** Mold and yeast forms depending on the temperature |
|||
** Best stain is GMS (Giemsa m…. silver) |
|||
** Seen within the macrophages |
|||
* Serology can be done for antigen or antibody |
|||
** Serology may be negative in immunosuppressed patients |
|||
** Antigen of '''urine''' (best), BAL fluid, and serum if available |
|||
*** Urine is best, but only 40% sensitive in cavitary, up to 95% in AIDS patients |
|||
*** Cross-reacts with other endemic fungi; false-positives with antithymocyte globulin |
|||
* PCR is possible |
|||
** 16S PCR |
|||
*Histopathology of biopsy specimens |
|||
== Management == |
|||
**Caseating and non-caseating granulomas |
|||
**Mold and yeast forms depending on the temperature |
|||
***Best stain is GMS (Gomori methenamine silver) |
|||
***Seen within the macrophages |
|||
*Fungal culture of sputum (chronic cavitary), or blood or bone marrow aspirate (disseminated), or CSF (CNS histo) |
|||
**Usually grows within 7 days, and almost always within 21 days |
|||
**Need to use lysis centrifugation system to release intracellular pathogens before culture |
|||
**Yield of 15% for acute pulmonary, but cavitary is 60% and up to 90% in advanced HIV with bronchoscopy |
|||
**Bone marrow and blood cultures are 50% sensitive |
|||
**Sensitivity increases with volume and number of samples |
|||
*Serology can be done for antigen or antibody |
|||
**Serology for antibodies by complement fixation |
|||
**Serology for antibodies by agar gel precipitin test |
|||
***Anti-H is uncommon (<10% of patients), but signifies active infection |
|||
***Anti-M is common (up to 80% of patients), but signifies either active or recovered infection |
|||
**Serology may be negative in immunosuppressed patients |
|||
**Antigen of '''urine''' (best), BAL fluid, and serum if available |
|||
***Urine is best, but only 40% sensitive in cavitary, up to 95% in AIDS patients |
|||
****However, this may no longer be the case, with overall sensitivity of 80% and specificity of 90% regardless of sample source |
|||
***Cross-reacts with other endemic fungi; false-positives with antithymocyte globulin |
|||
*PCR is possible |
|||
**16S PCR |
|||
==Management== |
|||
{| |
|||
! Syndrome |
|||
*In general, mild infections are treated with [[Is treated by::itraconazole]] and severe infections with [[Is treated by::amphotericin B]] |
|||
! Treatment |
|||
**Give tablets of [[itraconazole]] with acidic drink, such as can of soda, and avoid antacids |
|||
**[[Itraconazole]] requires therapeutic drug monitoring |
|||
*[[Is treated by::Voriconazole]] is an easier-to-prescribe alternative that is likely as effective as [[itraconazole]] |
|||
*Indications for antifungal therapy |
|||
**'''Definitely:''' moderate to severe acute diffuse pulmonary infection, chronic cavitary pulmonary disease, disseminated disease, CNS infection |
|||
**'''Possibly/uncertain:''' asymptomatic, mild symptoms lasting longer than 1 month, acute focal pulmonary infection, mediastinal lymphadenitis, mediastinal granuloma |
|||
**'''Not recommended:''' mediastinal fibrosis, pulmonary nodule, broncholithiasis, presumed ocular histoplasmosis syndrome |
|||
{| class="wikitable" |
|||
!Syndrome |
|||
!Treatment |
|||
|- |
|- |
||
| Acute pulmonary histoplasmosis |
| colspan="2" |'''Acute pulmonary histoplasmosis''' |
||
| |
|||
|- |
|- |
||
| |
| Mild, self-resolving |
||
| |
|If resolves within a month, no need to treat |
||
|- |
|- |
||
| |
| Mild, ongoing symptoms |
||
| |
|[[Itraconazole]] 200 mg po TID x3d then itra 200 mg po daily or BID for 6-12 weeks |
||
|- |
|- |
||
| |
| Moderate to severe |
||
| |
|[[Liposomal amphotericin B]] 3-5 mg/kg/d for 1-2 weeks, followed by [[itraconazole]] 200 mg TID x3d then [[itraconazole]] 200 mg BID x12wk<br />[[Methylprednisolone]] 0.5-1 mg/kg IV daily for first 1-2 weeks if respiratory complications |
||
|- |
|- |
||
| |
|Chronic cavitary pulmonary histoplasmosis |
||
| |
|[[Itraconazole]] 200 mg TID x3d then daily or BID for at least 1 year (18-24 months may have lower relapse) |
||
|- |
|- |
||
| Complications |
| colspan="2" |'''Complications''' |
||
| |
|||
|- |
|- |
||
| |
| Pericarditis |
||
| |
|NSAIDs if mild<br />[[Prednisone]] 0.5-1 mg/kg daily then taper over 1-2 weeks, plus [[itraconazole]] (as above) for 6-12 weeks if hemodynamic compromise<br />May need therapeutic pericardiocentesis |
||
|- |
|- |
||
| |
| Rheumatologic |
||
| |
|NSAIDs if mild, [[prednisone]] and [[itraconazole]] (as for pericarditis) if severe |
||
|- |
|- |
||
| |
| Mediastinal lymphadenitis |
||
| |
|Usually no treatment. Follow guide for acute pulmonary histoplasmosis. |
||
|- |
|- |
||
| |
| Mediastinal granuloma |
||
| |
|Usually no treatment. Standard [[itraconazole]] protocol for 6-12 weeks if symptomatic. |
||
|- |
|- |
||
| |
| [[Fibrosing mediastinitis|Mediastinal fibrosis]] |
||
| |
|Antifungals not recommended. Treat only if there is suspicion of mediastinal granuloma. May need stenting of obstructed pulmonary vessels. |
||
|- |
|- |
||
| |
| Broncholithiasis |
||
| |
|Antifungals not recommended. May need surgery. |
||
|- |
|- |
||
| |
|'''Progressive disseminated histoplasmosis''' |
||
| |
|Follow antigen levels during therapy and for 12 months after to monitor for relapse |
||
|- |
|- |
||
| |
| Mild to moderate |
||
| |
|[[Itraconazole]] for 12 months |
||
|- |
|- |
||
| |
| Moderately severe to severe |
||
| |
|[[Liposomal amphotericin B]] 3 mg/kg for 1-2 weeks then oral [[itraconazole]] for at least 12 months |
||
|- |
|- |
||
| |
| Immunosuppressed |
||
| |
|May need lifelong suppressive therapy with [[itraconazole]] 200 mg po daily |
||
|- |
|- |
||
| |
|CNS histoplasmosis |
||
| |
|[[Liposomal amphotericin B]] 5 mg/kg daily for 4-6 weeks (total 175 mg/kg) followed by itraconazole for at least 1 year, until resolution of CSF abnormalities |
||
|- |
|- |
||
| |
|Pregnancy |
||
| |
|[[Liposomal amphotericin B]] 3-5 mg/kg for 4-6 weeks |
||
|- |
|- |
||
| |
|Children |
||
| |
|As per above guidelines, with [[amphotericin B deoxycholate]] 1 mg/kg and [[itraconazole]] 2.5-5 mg/kg bid (max 400 mg daily) |
||
|- |
|- |
||
| |
|Prophylaxis |
||
| |
|[[Itraconazole]] 200 mg po daily recommended if [[HIV]] with CD4 <150 and more than 10 cases per 100 patient-years |
||
|} |
|} |
||
'''Note:''' therapeutic drug level monitoring is recommended for itraconazole |
*'''Note:''' therapeutic drug level monitoring is recommended for itraconazole |
||
*'''Source:''' IDSA guidelines 2007 |
|||
==Prevention== |
|||
===Lab Safety=== |
|||
*[[Biosafety risk groups|Biosafety risk group 3]] organism, so needs BSL 3 |
|||
*Should be suspected with any white mold |
|||
===Prophylaxis=== |
|||
'''Source:''' IDSA guidelines 2007 |
|||
*May be indicated for endemic areas in patients with advanced HIV and low CD4 count |
|||
{{DISPLAYTITLE:''Histoplasma capsulatum''}} |
{{DISPLAYTITLE:''Histoplasma capsulatum''}} |
||
[[Category:Dimorphic fungi]] |
[[Category:Dimorphic fungi]] |
||
Latest revision as of 15:05, 29 October 2020
Background
Microbiology
- Saprophytic environmental fungus withing the family Ascomycetes
- Thermally dimorphic, existing as a mold <35ºC and a yeast at >37ºC
- Mold
- Mold form is highly infectious, associated with lab-related outbreaks
- Septate hyaline mold with aerial hyphae with macroconidia, which are its identifying feature
- Two types of conidia: tuberculate macroconidia (ovoid bodies 8 to 15 μm with spikes), and microconidia (small, smooth oval bodies 2 to 5 μm)
- Two colony types, brown (B) and albino (A)
- Yeast
- Non-infectious, once hanging out in your body
- Small, 2 to 5 μm
- Demonstrates multipolar narrow-based budding
- Does not look particularly different from other yeast, but may be intracellular
- Mold
- Three variants
- H. capsulatum var. capsulatum, which is the most common worldwide, and is further divided into various clades
- H. capsulatum var. duboisii which is only present in western Africa, and has larger yeast forms
- Can take up to 7 days to grow
- H. capsulatum var. farciminosum
Epidemiology
- Endemic in many parts of the world
- Ohio and Mississippi River Valley systems (Central/Eastern US), where seroprevalence is as high as 80% in adults
- Probably up through St. Lawrence River as well
- Probably more broadly distributed, including Central and South America, South and East Asia, and Australia
- H. capsulatum var. duboisii in western Africa
- Typically found in moist soil enriched with bat or bird droppings, which helps it to sporulate
- Disturbing the soil aerosolizes it, allowing the microconidia to be inhaled
- Microconidia can be transported for miles by air currents
Risk Factors
- HIV, solid organ transplant, hematologic transplant
- Primary immunodeficiencies: X-linked hypogammaglobulinemia
Pathophysiology
- Inhaled microconidia reach the alveolii and are phagocytosed by alveolar macrophages
- Innoculum size can be smaller with immunodeficiency
- Size of innoculation affects disease severity and progression
- Microconidia transform into budding yeasts, in a process that is dependent on intracellular macrophage calcium and iron
- They multiply inside macrophages, and translocate through the lymphatics
- Cellular immunity developed around 2 weeks later
- Response depends on IL-12 and TNF-α
- Organize to form granulomas to contain the infection
- Latent infection can reactivate, but rare
- Most common with infliximab
- In impaired cellular immunity, infection can become disseminated
Clinical Manifestations
- Spectrum of illness, related to the size of the inoculum, strain-specific virulence, and host immunity
- Often asymptomatic; in endemic areas, 50-80% of people skin-test positive or have radiographic evidence of previous infection
- Can cross tissue planes
Acute Pulmonary Histoplasmosis
- Fever, chill, malaise, headaches, myalgias, anorexia, cough, dyspnea, and chest pain
- Spectrum from mild to severe
- Usually self-limited, no need to treat unless longer than a month
- Pneumonitis on chest x-ray, often with adenopathy
- "Buckshot" appearance? (Mandell)
- Can have rheumatologic sequelae in 5-10%, with arthralgias, arthritis, and erythema nodosum
- Can have pericarditis from the inflammatory response
- Hilar adenopathy can necrotize
Progressive Disseminated Histoplasmosis
- Usually, though not exclusively, in immunocompromised patients
- Risk factors include CD4 <200, very old or very young, and therapeutic immunosuppression (prednisone, MMF, tacrolimus, methotrexate, TNF-α inhibitors, other biologics)
- Can be rapidly-progressing and acute, or more subacute
Acute Progressive Disseminated Histoplasmosis
- Fever, weight loss, organomegaly, thrombocytopenia
- Meningitis or focal brain lesions
- Oral and GI mucosal ulcerations
- Adrenal insufficiency
Chronic Progressive Disseminated Histoplasmosis
- In normal hosts
- Absent or low-grade fever
- Longer course
- Most common finding is oropharyngeal lesion: deep, well-circumscribed, unrated, and painless
- Mimics squamous cell carcinoma
- Can also have hepatosplenomegaly, chronic meningitis, or chronic granulomatous hepatitis
Chronic Cavitary Histoplasmosis
- Typically seen in bullous emphysema
- Productive cough, dyspnea, low-grade fever, night sweats, weight loss
- Hemoptysis is rare
- Progressive without treatment
- Chest x-ray shows upper-lobe infiltrations, vacitation, and pleural thickening, similar to tuberculosis
Fibrosing Mediastinitis
- Histoplasmosis is the most common cause of fibrosing mediastinitis
- Rare but serious
- Progressive fibrosis around hilar/mediastinal lymphadenopathy, wither unilateral or bilateral
- Occludes central vessels and airways
- Can present with a SVC syndrome, obstruction of pulmonary vessels, or airway obstruction
- Can also present with recurrent pneumonias, hemoptysis, or respiratory failure
- 30% mortality
Other Complications
- Ophthalmic posterior uveitis
- Meningitis
- Infective endocarditis
African Histoplasmosis
- H. capsulatum vars. capsulatum and duboisii coexist in Africa
- var. duboisii has more skin and skeletal manifestations
- Ulcers, nodules, or psoriaform lesions that can spontaneously resolve
- Can cause a cold abscess, without inflammation
- Osteolytic bone lesions are common (50%) of cases
- Skull and ribs most common
- Can have sinus formation and cystic bone lesions
- May not have any evidence on CXR of prior pulmonary histoplasmosis
- Can also present with progressive disseminated disease, with fevers and multiorgan involvement
- Combianation of granulomas and pus
- Larger yeast is harder for macrophages to engulf
- Ulcers, nodules, or psoriaform lesions that can spontaneously resolve
Diagnosis
- Histopathology of biopsy specimens
- Caseating and non-caseating granulomas
- Mold and yeast forms depending on the temperature
- Best stain is GMS (Gomori methenamine silver)
- Seen within the macrophages
- Fungal culture of sputum (chronic cavitary), or blood or bone marrow aspirate (disseminated), or CSF (CNS histo)
- Usually grows within 7 days, and almost always within 21 days
- Need to use lysis centrifugation system to release intracellular pathogens before culture
- Yield of 15% for acute pulmonary, but cavitary is 60% and up to 90% in advanced HIV with bronchoscopy
- Bone marrow and blood cultures are 50% sensitive
- Sensitivity increases with volume and number of samples
- Serology can be done for antigen or antibody
- Serology for antibodies by complement fixation
- Serology for antibodies by agar gel precipitin test
- Anti-H is uncommon (<10% of patients), but signifies active infection
- Anti-M is common (up to 80% of patients), but signifies either active or recovered infection
- Serology may be negative in immunosuppressed patients
- Antigen of urine (best), BAL fluid, and serum if available
- Urine is best, but only 40% sensitive in cavitary, up to 95% in AIDS patients
- However, this may no longer be the case, with overall sensitivity of 80% and specificity of 90% regardless of sample source
- Cross-reacts with other endemic fungi; false-positives with antithymocyte globulin
- Urine is best, but only 40% sensitive in cavitary, up to 95% in AIDS patients
- PCR is possible
- 16S PCR
Management
- In general, mild infections are treated with itraconazole and severe infections with amphotericin B
- Give tablets of itraconazole with acidic drink, such as can of soda, and avoid antacids
- Itraconazole requires therapeutic drug monitoring
- Voriconazole is an easier-to-prescribe alternative that is likely as effective as itraconazole
- Indications for antifungal therapy
- Definitely: moderate to severe acute diffuse pulmonary infection, chronic cavitary pulmonary disease, disseminated disease, CNS infection
- Possibly/uncertain: asymptomatic, mild symptoms lasting longer than 1 month, acute focal pulmonary infection, mediastinal lymphadenitis, mediastinal granuloma
- Not recommended: mediastinal fibrosis, pulmonary nodule, broncholithiasis, presumed ocular histoplasmosis syndrome
| Syndrome | Treatment |
|---|---|
| Acute pulmonary histoplasmosis | |
| Mild, self-resolving | If resolves within a month, no need to treat |
| Mild, ongoing symptoms | Itraconazole 200 mg po TID x3d then itra 200 mg po daily or BID for 6-12 weeks |
| Moderate to severe | Liposomal amphotericin B 3-5 mg/kg/d for 1-2 weeks, followed by itraconazole 200 mg TID x3d then itraconazole 200 mg BID x12wk Methylprednisolone 0.5-1 mg/kg IV daily for first 1-2 weeks if respiratory complications |
| Chronic cavitary pulmonary histoplasmosis | Itraconazole 200 mg TID x3d then daily or BID for at least 1 year (18-24 months may have lower relapse) |
| Complications | |
| Pericarditis | NSAIDs if mild Prednisone 0.5-1 mg/kg daily then taper over 1-2 weeks, plus itraconazole (as above) for 6-12 weeks if hemodynamic compromise May need therapeutic pericardiocentesis |
| Rheumatologic | NSAIDs if mild, prednisone and itraconazole (as for pericarditis) if severe |
| Mediastinal lymphadenitis | Usually no treatment. Follow guide for acute pulmonary histoplasmosis. |
| Mediastinal granuloma | Usually no treatment. Standard itraconazole protocol for 6-12 weeks if symptomatic. |
| Mediastinal fibrosis | Antifungals not recommended. Treat only if there is suspicion of mediastinal granuloma. May need stenting of obstructed pulmonary vessels. |
| Broncholithiasis | Antifungals not recommended. May need surgery. |
| Progressive disseminated histoplasmosis | Follow antigen levels during therapy and for 12 months after to monitor for relapse |
| Mild to moderate | Itraconazole for 12 months |
| Moderately severe to severe | Liposomal amphotericin B 3 mg/kg for 1-2 weeks then oral itraconazole for at least 12 months |
| Immunosuppressed | May need lifelong suppressive therapy with itraconazole 200 mg po daily |
| CNS histoplasmosis | Liposomal amphotericin B 5 mg/kg daily for 4-6 weeks (total 175 mg/kg) followed by itraconazole for at least 1 year, until resolution of CSF abnormalities |
| Pregnancy | Liposomal amphotericin B 3-5 mg/kg for 4-6 weeks |
| Children | As per above guidelines, with amphotericin B deoxycholate 1 mg/kg and itraconazole 2.5-5 mg/kg bid (max 400 mg daily) |
| Prophylaxis | Itraconazole 200 mg po daily recommended if HIV with CD4 <150 and more than 10 cases per 100 patient-years |
- Note: therapeutic drug level monitoring is recommended for itraconazole
- Source: IDSA guidelines 2007
Prevention
Lab Safety
- Biosafety risk group 3 organism, so needs BSL 3
- Should be suspected with any white mold
Prophylaxis
- May be indicated for endemic areas in patients with advanced HIV and low CD4 count