Blastomyces dermatitidis: Difference between revisions
From IDWiki
Blastomyces dermatitidis
No edit summary |
No edit summary |
||
| (10 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| + | ==Background== |
||
| − | = Microbiology = |
||
| + | ===Microbiology=== |
||
| − | * |
+ | *Broad-based dimorphic budding yeast |
| − | * |
+ | *Mold at 25-28ºC and yeast at 37ºC |
| − | * |
+ | *Branching hyphae 2-3 µm in diameter and right-angle conidiophores resembling lollipops |
| − | ** |
+ | **Conidia become airborne when disturbed |
| − | = |
+ | ===Epidemiology=== |
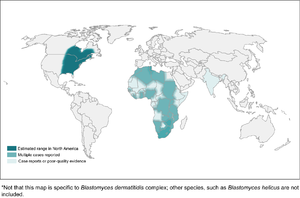
| + | [[File:Blastomycosis_map.png|thumb|Distribution of blastomycosis]] |
||
| − | * Present in the Mississippi, Ohio, and St. Lawrence River Valleys, the Great Lakes regions, and western Ontario |
||
| + | *Present in the Mississippi, Ohio, and St. Lawrence River Valleys, the Great Lakes regions, and western Ontario |
||
| − |  |
||
| + | *May also be endemic to Africa and India, though it's unclear whether these are true cases or late reactivation |
||
| + | *Hosts include humans, dogs, cats, horses, brown bears, and exotic pets like the kinkajou and red ruffed lemur |
||
| + | *There have been point-source outbreaks associated with occupational and recreational activities, usually along streams or rivers enriched with decaying vegetation |
||
| + | *Possibly has cold-weather seasonality |
||
| + | ===Pathophysiology=== |
||
| − | * May also be endemic to Africa and India, though it's unclear whether these are true cases or late reactivation |
||
| − | * Hosts include humans, dogs, cats, horses, brown bears, and exotic pets like the kinkajou and red ruffed lemur |
||
| − | * There have been point-source outbreaks associated with occupational and recreational activities, usually along streams or rivers enriched with decaying vegetation |
||
| − | * Possibly has cold-weather seasonality |
||
| + | *Inhalation of conidia into the lungs |
||
| − | = Pathophysiology = |
||
| + | *Macophages can phagocytize and kill the conidia, and can also slow conversion into yeast form |
||
| + | **A thick cell wall helps to prevent phagocytosis |
||
| + | *Some conidia successfully convert to the pathogenic yeast form |
||
| + | *Major antigens include BAD1 on the cell wall surface and binds CR3 (CD11b/CD18) and CD14 |
||
| + | *Humoral immunity has little effect; rather, immune response relies on cell-mediated immunity |
||
| + | ==Clinical Manifestations== |
||
| − | * Inhalation of conidia into the lungs |
||
| − | * Macophages can phagocytize and kill the conidia, and can also slow conversion into yeast form |
||
| − | ** A thick cell wall helps to prevent phagocytosis |
||
| − | * Some conidia successfully convert to the pathogenic yeast form |
||
| − | * Major antigens include BAD1 on the cell wall surface and binds CR3 (CD11b/CD18) and CD14 |
||
| − | * Humoral immunity has little effect; rather, immune response relies on cell-mediated immunity |
||
| + | *Can be acute pneumonia (followed by either recovery or chronic infection), or asymptomatic (followed by recovery or chronic infection) |
||
| − | = Clinical Presentation = |
||
| + | **About 50% overall resolve without treatment |
||
| + | **About half of symptomatic patients have isolated lung involvement and half are disseminated |
||
| + | *When symptomatic, may have non-specific and constitutional symptoms |
||
| + | *Can be primary or reactivation |
||
| + | *Incubation period [[Usual incubation period::3 weeks to 3 months]] |
||
| + | ===Respiratory Blastomycosis=== |
||
| − | * Can be acute pneumonia (followed by either recovery or chronic infection), or asymptomatic (followed by recovery or chronic infection) |
||
| − | ** About 50% overall resolve without treatment |
||
| − | ** About half of symptomatic patients have isolated lung involvement and half are disseminated |
||
| − | * When symptomatic, may have non-specific and constitutional symptoms |
||
| − | * Can be primary or reactivation |
||
| − | * Incubation period 3 weeks to 3 months |
||
| − | + | *Respiratory symptoms are the most common focus |
|
| + | *Can mimic community-acquired pneumonia or tuberculosis, and may have hemoptysis |
||
| + | **Less likely cavitary, but possible |
||
| + | *Can be acute or chronic presentation, or asymptomatic |
||
| + | **Chronic typically lasts 2 to 6 months, with constitutional symptoms |
||
| + | *Even if there is non-pulmonary infection, there are often findings on chest x-ray |
||
| + | *Can also cause ARDS in about 10% of cases, which distinguishes it from histoplasmosis |
||
| + | ===Extra-Pulmonary Blastomycosis=== |
||
| − | * Respiratory symptoms are the most common focus |
||
| − | * Can mimic community-acquired pneumonia or tuberculosis, and may have hemoptysis |
||
| − | ** Less likely cavitary, but possible |
||
| − | * Can be acute or chronic presentation, or asymptomatic |
||
| − | ** Chronic typically lasts 2 to 6 months, with constitutional symptoms |
||
| − | * Even if there is non-pulmonary infection, there are often findings on chest x-ray |
||
| − | * Can also cause ARDS in about 10% of cases, which distinguishes it from histoplasmosis |
||
| + | *Next most common feature is dissemination to skin |
||
| − | == Extra-pulmonary blastomycosis == |
||
| + | **Lesions usually either verrucous or ulcerative |
||
| + | **May be misdiagnosed as pyoderma gangrenosum, keratoacanthoma, BCC, squamous cell carcinoma, or mycosis fungoides |
||
| + | **Differential also contains NTM, other fungal infections, lupus |
||
| + | *Osteomyelitis, with or without evidence of lung involvement, is the third most common form |
||
| + | **There are no specific clinical or radiographical features of blastomycosis |
||
| + | *Genitourinary involvement, especially prostatitis and epididymo-orchitis, are next most common |
||
| + | **May be cultured in urine collected after prostate massage |
||
| + | *Meningitis and cerebritis/abscess are possible |
||
| + | **Consider screening for it in immunocompromised people |
||
| + | **Cerebellum more common |
||
| + | **CSF culture is insenitive, though PCR is better |
||
| + | **Found in 5-10% of cases of disseminated blasto, but associated with high mortality |
||
| + | **Can have ocular involvement, as well |
||
| + | **Differential would involve bacterial and fungal meningitis/abscess (including cryptococcosis), and Nocardia |
||
| + | *Can also affect larynx, lymphatics or lymph nodes, spleen, and any other organ, though fungemia is rarely found |
||
| + | *Infection can cause endocrinologic abnormalities including adrenal insufficiency, thyroid infection, hypercalcemia (granulomatous) |
||
| + | **There are case reports of diabetes insipidus, and hyperprolactinemia |
||
| + | *Because it can occur in any organ, there are also case reports of breast lesions, tubo-ovarian abscess, otitis media, branchial cleft cyst infection |
||
| + | ===Pregnancy=== |
||
| − | * Next most common feature is dissemination to skin |
||
| − | ** Lesions usually either verrucous or ulcerative |
||
| − | ** May be misdiagnosed as pyoderma gangrenosum, keratoacanthoma, BCC, squamous cell carcinoma, or mycosis fungoides |
||
| − | ** Differential also contains NTM, other fungal infections, lupus |
||
| − | * Osteomyelitis, with or without evidence of lung involvement, is the third most common form |
||
| − | ** There are no specific clinical or radiographical features of blastomycosis |
||
| − | * Genitourinary involvement, especially prostatitis and epididymo-orchitis, are next most common |
||
| − | ** May be cultured in urine collected after prostate massage |
||
| − | * Meningitis and cerebritis/abscess are possible |
||
| − | ** Consider screening for it in immunocompromised people |
||
| − | ** Cerebellum more common |
||
| − | ** CSF culture is insenitive, though PCR is better |
||
| − | ** Found in 5-10% of cases of disseminated blasto, but associated with high mortality |
||
| − | ** Can have ocular involvement, as well |
||
| − | ** Differential would involve bacterial and fungal meningitis/abscess (including cryptococcosis), and Nocardia |
||
| − | * Can also affect larynx, lymphatics or lymph nodes, spleen, and any other organ, though fungemia is rarely found |
||
| − | * Infection can cause endocrinologic abnormalities including adrenal insufficiency, thyroid infection, hypercalcemia (granulomatous) |
||
| − | ** There are case reports of diabetes insipidus, and hyperprolactinemia |
||
| − | * Because it can occur in any organ, there are also case reports of breast lesions, tubo-ovarian abscess, otitis media, branchial cleft cyst infection |
||
| + | *May be higher risk group, and can transmit it to the newborn |
||
| − | == Pregnancy == |
||
| + | ===Immunocompromised Patients=== |
||
| − | * May be higher risk group, and can transmit it to the newborn |
||
| + | *Not as commonly described as an opportunistic infection as the other endemic fungi |
||
| − | == Immunocompromise == |
||
| + | *Few cases with advanced [[HIV]], but possible |
||
| + | *[[Sarcoidosis]], [[transplantation]], and [[Corticosteroids|steroid]] use are all risk factors |
||
| + | *[[Infliximab]] and [[etanercept]] are higher risk |
||
| + | ==Diagnosis== |
||
| − | * Not as commonly described as an opportunistic infection as the other endemic fungi |
||
| − | * Few cases with AIDS, but possible |
||
| − | * Sarcoidosis, transplantation, and steroid use are all risk factors |
||
| − | * Infliximab and etanercept are higher risk |
||
| + | *Requires a microbiologic diagnosis |
||
| − | = Diagnosis = |
||
| + | ===Microscopy=== |
||
| − | * Requires a microbiologic diagnosis |
||
| + | *Can be directly visualized on exudate, sputum, tissue, or really any sample |
||
| − | == Microscopy == |
||
| + | *Fairly easy to see with KOH or calcofluor |
||
| + | *Can be seen on histology of skin lesion biopsy with Gomori methenamine silver (GMS) and periodic acid-Schiff (PAS) stains |
||
| + | *Thick-walled, multinucleated, broad-based budding |
||
| + | ===Culture=== |
||
| − | * Can be directly visualized on exudate, sputum, tissue, or really any sample |
||
| − | * Fairly easy to see with KOH or calcofluor |
||
| − | * Can be seen on histology of skin lesion biopsy with Gomori methenamine silver (GMS) and periodic acid-Schiff (PAS) stains |
||
| − | * Thick-walled, multinucleated, broad-based budding |
||
| + | *Grows as mycelial (mold) form at 25-30ºC, usually after 1 to 3 weeks, starting as a white mold that slowly turns light brown |
||
| − | == Culture == |
||
| + | **Grows 5-10 days before they develop conidia, so relatively low risk of infection early on |
||
| + | *Usually needs a DNA probe to confirm the species |
||
| + | *Biosafety level 3 pathogen, so needs to be sent to Public Health |
||
| + | ===Serology=== |
||
| − | * Grows as mycelial (mold) form at 25-30ºC, usually after 1 to 3 weeks, starting as a white mold that slowly turns light brown |
||
| − | ** Grows 5-10 days before they develop conidia, so relatively low risk of infection early on |
||
| − | * Usually needs a DNA probe to confirm the species |
||
| − | * Biosafety level 3 pathogen, so needs to be sent to Public Health |
||
| + | *Antibody |
||
| − | == Serology == |
||
| + | **Serology with complement fixation is insensitive |
||
| + | **A antigen antibodies is better (Sn 65-80%, Sp 100%) |
||
| + | **BAD1 antigen antibodies is 85% sensitive but not yet used |
||
| + | *Urinary antigen has 93% sens and 80% spec |
||
| + | **It cross-reacts with other dimorphic fungi, especially histoplasmosis |
||
| + | **Can be trended to monitor response during therapy |
||
| + | *Can check 1,3-β-d-glucan, but not specific or particularly sensitive |
||
| + | ===Molecular Methods=== |
||
| − | * Antibody |
||
| − | ** Serology with complement fixation is insensitive |
||
| − | ** A antigen antibodies is better (Sn 65-80%, Sp 100%) |
||
| − | ** BAD1 antigen antibodies is 85% sensitive but not yet used |
||
| − | * Urinary antigen has 93% sens and 80% spec |
||
| − | ** It cross-reacts with other dimorphic fungi, especially histoplasmosis |
||
| − | ** Can be trended to monitor response during therapy |
||
| − | * Can check 1,3-β-d-glucan, but not specific or particularly sensitive |
||
| + | *Not yet well-developed, but theoretically possible to do PCR |
||
| − | == Molecular methods == |
||
| + | ==Management== |
||
| − | * Not yet well-developed, but theoretically possible to do PCR |
||
| + | *Chronic blastomycosis doesn't resolve without treatment, and mortality is as high as 60% |
||
| − | = Management = |
||
| + | *Although many cases of acute pulmonary blastomycosis self-resolve, it is still recommended to treat, since triazoles are well-tolerated |
||
| + | *Severity is based on clinical judgement, as there are no validated criteria |
||
| + | ===Pulmonary Blastomycosis=== |
||
| − | * Chronic blasto doesn't resolve without treatment, and mortality is as high as 60% |
||
| − | * Although many cases of acute pulmonary blasto self-resolve, it is still recommended to treat, since azoles are well-tolerated |
||
| − | * Severity is based on clinical judgement, as there are no validated criteria |
||
| − | * Pulmonary blastomycosis |
||
| − | ** Mild-to-moderate: itraconazole 200 mg po tid for 3 days followed by bid for 6-12 months |
||
| − | ** Moderate severe-to-severe: liposomal amphotericin B 3-5 mg/kg per day for 1-2 weeks or until improvement, followed by itraconazole 200 mg po tid for 3 days, followed by itraconazole 200 mg po bid, for a total of 6 to 12 months |
||
| − | *** May need 6 to 8 weeks of induction |
||
| − | ** Monitor serum itraconazole after 2 weeks |
||
| − | * Disseminated extrapulmonary blastomycosis |
||
| − | ** Same as for pulmonary blastomycosis |
||
| − | ** 12 months for bone and CNS involvement |
||
| − | * CNS blastomycosis |
||
| − | ** Amphotericin 5 mg/kg per day for 4-6 weeks followed by an azole for at least 12 months and until resolution of CSF abnormalities |
||
| − | ** Azoles include fluconazole 800 mg daily, itraconazole 200 mg bid or tid, or voriconazole 200-300 mg bid |
||
| − | *** Vori ''may'' be better for CNS disease |
||
| − | * Immunosuppressed patients with blastomycosis, including AIDS |
||
| − | ** Same as for severe pulmonary blastomycosis, but duration is at least 12 months |
||
| − | ** May be followed by lifelong suppressive itraconazole 200 mg po daily if immunosuppression cannot be decreased and they have relapsed despite appropriate therapy |
||
| − | * Blastomycosis in pregnant women |
||
| − | ** Use liposomal amphotericin 3-5 mg/kg per day |
||
| − | ** Avoid azoles for risk of teratogenicity |
||
| − | * Blastomycosis in newborns: AmB deoxycholate 1 mg/kg per day |
||
| − | * Blastomycosis in children |
||
| − | ** Mild-to-moderate: itraconazole 10 mg/kg po per day (up to 400 mg) for 6 to 12 months |
||
| − | ** Severe blastomycosis: AmB deoxycholate 0.7-1 mg/kg per day or liposomal AmB at 3-5 mg/kg per day, followed by itraconazole 10 mg/kg po per day (up to 400 mg), for a total of 12 months |
||
| − | ** Monitor serum levels after 2 weeks |
||
| + | *Mild-to-moderate: [[Is treated by::itraconazole]] 200 mg po tid for 3 days followed by bid for 6-12 months |
||
| − | == Itraconazole == |
||
| + | *Moderate severe-to-severe: [[Is treated by::liposomal amphotericin B]] 3-5 mg/kg per day for 1-2 weeks or until improvement, followed by [[itraconazole]] 200 mg po tid for 3 days, followed by [[itraconazole]] 200 mg po bid, for a total of 6 to 12 months |
||
| + | **May need up 6 to 8 weeks of induction with [[liposomal amphotericin B]] |
||
| + | *Monitor serum [[itraconazole]] after 2 weeks, targeting 1 to 10 μg/mL |
||
| + | ===Disseminated Extrapulmonary Blastomycosis=== |
||
| − | * Tablet formulation has poorer oral bioavailability than liquid formulation |
||
| − | * Need to avoid PPI and H2 blockers, as it needs an acidic stomach environment to get absorbed, especially for tablet formulation |
||
| − | * Not as good CNS penetration as other azoles |
||
| − | * Needs therapeutic drug monitoring after 2 weeks with goal of maintaining serum levels between 1.0 and 10.0 g/ml |
||
| + | *Same as for pulmonary blastomycosis, but treated for at least 12 months if bone involvement |
||
| − | = Further Reading = |
||
| + | ===CNS Blastomycosis=== |
||
| − | * Chapman SW ''et al.'' [https://doi.org/10.1086/588300 Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America]. ''Clin Infect Dis''. 2008 46(12):1801-1812. |
||
| + | |||
| + | *[[Is treated by::Amphotericin B]] 5 mg/kg per day for 4-6 weeks followed by an azole for at least 12 months and until resolution of CSF abnormalities |
||
| + | *Azoles include [[Is treated by::fluconazole]] 800 mg daily, [[Is treated by::itraconazole]] 200 mg bid or tid, or [[Is treated by::voriconazole]] 200-300 mg bid |
||
| + | **[[Voriconazole]] ''may'' be better for CNS disease (better CNS penetration than [[itraconazole]], and very good in vitro activity) |
||
| + | |||
| + | ===Immunocompromised Patients=== |
||
| + | |||
| + | *Same as for severe pulmonary blastomycosis, but duration is at least 12 months |
||
| + | *May be followed by lifelong suppressive [[Is treated by::itraconazole]] 200 mg po daily if immunosuppression cannot be decreased and they have relapsed despite appropriate therapy |
||
| + | |||
| + | ===Pregnant women=== |
||
| + | |||
| + | *Use [[Is treated by::liposomal amphotericin B]] 3-5 mg/kg per day |
||
| + | *Avoid azoles for risk of teratogenicity |
||
| + | |||
| + | ===Children=== |
||
| + | |||
| + | *Blastomycosis in newborns: [[Is treated by::amphotericin B deoxycholate]] 1 mg/kg per day |
||
| + | *Blastomycosis in children |
||
| + | **Mild-to-moderate: [[Is treated by::itraconazole]] 10 mg/kg po per day (up to 400 mg) for 6 to 12 months |
||
| + | **Severe blastomycosis: [[Is treated by::amphotericin B deoxycholate]] 0.7-1 mg/kg per day or [[Is treated by::liposomal amphotericin B]] at 3-5 mg/kg per day, followed by [[itraconazole]] 10 mg/kg po per day (up to 400 mg), for a total of 12 months |
||
| + | **Monitor serum levels after 2 weeks |
||
| + | |||
| + | ===Itraconazole=== |
||
| + | |||
| + | *Tablet formulation has poorer oral bioavailability than liquid formulation |
||
| + | *Need to avoid [[PPIs]] and [[H2 blockers]], as it needs an acidic stomach environment to get absorbed, especially for tablet formulation |
||
| + | *Not as good CNS penetration as other [[triazoles]] |
||
| + | *Needs therapeutic drug monitoring after 2 weeks with goal of maintaining serum levels between 1.0 and 10.0 μg/ml |
||
| + | |||
| + | ==Further Reading== |
||
| + | |||
| + | *Chapman SW ''et al.'' [https://doi.org/10.1086/588300 Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America]. ''Clin Infect Dis''. 2008 46(12):1801-1812. |
||
{{DISPLAYTITLE:''Blastomyces dermatitidis''}} |
{{DISPLAYTITLE:''Blastomyces dermatitidis''}} |
||
Latest revision as of 13:20, 14 September 2020
Background
Microbiology
- Broad-based dimorphic budding yeast
- Mold at 25-28ºC and yeast at 37ºC
- Branching hyphae 2-3 µm in diameter and right-angle conidiophores resembling lollipops
- Conidia become airborne when disturbed
Epidemiology
- Present in the Mississippi, Ohio, and St. Lawrence River Valleys, the Great Lakes regions, and western Ontario
- May also be endemic to Africa and India, though it's unclear whether these are true cases or late reactivation
- Hosts include humans, dogs, cats, horses, brown bears, and exotic pets like the kinkajou and red ruffed lemur
- There have been point-source outbreaks associated with occupational and recreational activities, usually along streams or rivers enriched with decaying vegetation
- Possibly has cold-weather seasonality
Pathophysiology
- Inhalation of conidia into the lungs
- Macophages can phagocytize and kill the conidia, and can also slow conversion into yeast form
- A thick cell wall helps to prevent phagocytosis
- Some conidia successfully convert to the pathogenic yeast form
- Major antigens include BAD1 on the cell wall surface and binds CR3 (CD11b/CD18) and CD14
- Humoral immunity has little effect; rather, immune response relies on cell-mediated immunity
Clinical Manifestations
- Can be acute pneumonia (followed by either recovery or chronic infection), or asymptomatic (followed by recovery or chronic infection)
- About 50% overall resolve without treatment
- About half of symptomatic patients have isolated lung involvement and half are disseminated
- When symptomatic, may have non-specific and constitutional symptoms
- Can be primary or reactivation
- Incubation period 3 weeks to 3 months
Respiratory Blastomycosis
- Respiratory symptoms are the most common focus
- Can mimic community-acquired pneumonia or tuberculosis, and may have hemoptysis
- Less likely cavitary, but possible
- Can be acute or chronic presentation, or asymptomatic
- Chronic typically lasts 2 to 6 months, with constitutional symptoms
- Even if there is non-pulmonary infection, there are often findings on chest x-ray
- Can also cause ARDS in about 10% of cases, which distinguishes it from histoplasmosis
Extra-Pulmonary Blastomycosis
- Next most common feature is dissemination to skin
- Lesions usually either verrucous or ulcerative
- May be misdiagnosed as pyoderma gangrenosum, keratoacanthoma, BCC, squamous cell carcinoma, or mycosis fungoides
- Differential also contains NTM, other fungal infections, lupus
- Osteomyelitis, with or without evidence of lung involvement, is the third most common form
- There are no specific clinical or radiographical features of blastomycosis
- Genitourinary involvement, especially prostatitis and epididymo-orchitis, are next most common
- May be cultured in urine collected after prostate massage
- Meningitis and cerebritis/abscess are possible
- Consider screening for it in immunocompromised people
- Cerebellum more common
- CSF culture is insenitive, though PCR is better
- Found in 5-10% of cases of disseminated blasto, but associated with high mortality
- Can have ocular involvement, as well
- Differential would involve bacterial and fungal meningitis/abscess (including cryptococcosis), and Nocardia
- Can also affect larynx, lymphatics or lymph nodes, spleen, and any other organ, though fungemia is rarely found
- Infection can cause endocrinologic abnormalities including adrenal insufficiency, thyroid infection, hypercalcemia (granulomatous)
- There are case reports of diabetes insipidus, and hyperprolactinemia
- Because it can occur in any organ, there are also case reports of breast lesions, tubo-ovarian abscess, otitis media, branchial cleft cyst infection
Pregnancy
- May be higher risk group, and can transmit it to the newborn
Immunocompromised Patients
- Not as commonly described as an opportunistic infection as the other endemic fungi
- Few cases with advanced HIV, but possible
- Sarcoidosis, transplantation, and steroid use are all risk factors
- Infliximab and etanercept are higher risk
Diagnosis
- Requires a microbiologic diagnosis
Microscopy
- Can be directly visualized on exudate, sputum, tissue, or really any sample
- Fairly easy to see with KOH or calcofluor
- Can be seen on histology of skin lesion biopsy with Gomori methenamine silver (GMS) and periodic acid-Schiff (PAS) stains
- Thick-walled, multinucleated, broad-based budding
Culture
- Grows as mycelial (mold) form at 25-30ºC, usually after 1 to 3 weeks, starting as a white mold that slowly turns light brown
- Grows 5-10 days before they develop conidia, so relatively low risk of infection early on
- Usually needs a DNA probe to confirm the species
- Biosafety level 3 pathogen, so needs to be sent to Public Health
Serology
- Antibody
- Serology with complement fixation is insensitive
- A antigen antibodies is better (Sn 65-80%, Sp 100%)
- BAD1 antigen antibodies is 85% sensitive but not yet used
- Urinary antigen has 93% sens and 80% spec
- It cross-reacts with other dimorphic fungi, especially histoplasmosis
- Can be trended to monitor response during therapy
- Can check 1,3-β-d-glucan, but not specific or particularly sensitive
Molecular Methods
- Not yet well-developed, but theoretically possible to do PCR
Management
- Chronic blastomycosis doesn't resolve without treatment, and mortality is as high as 60%
- Although many cases of acute pulmonary blastomycosis self-resolve, it is still recommended to treat, since triazoles are well-tolerated
- Severity is based on clinical judgement, as there are no validated criteria
Pulmonary Blastomycosis
- Mild-to-moderate: itraconazole 200 mg po tid for 3 days followed by bid for 6-12 months
- Moderate severe-to-severe: liposomal amphotericin B 3-5 mg/kg per day for 1-2 weeks or until improvement, followed by itraconazole 200 mg po tid for 3 days, followed by itraconazole 200 mg po bid, for a total of 6 to 12 months
- May need up 6 to 8 weeks of induction with liposomal amphotericin B
- Monitor serum itraconazole after 2 weeks, targeting 1 to 10 μg/mL
Disseminated Extrapulmonary Blastomycosis
- Same as for pulmonary blastomycosis, but treated for at least 12 months if bone involvement
CNS Blastomycosis
- Amphotericin B 5 mg/kg per day for 4-6 weeks followed by an azole for at least 12 months and until resolution of CSF abnormalities
- Azoles include fluconazole 800 mg daily, itraconazole 200 mg bid or tid, or voriconazole 200-300 mg bid
- Voriconazole may be better for CNS disease (better CNS penetration than itraconazole, and very good in vitro activity)
Immunocompromised Patients
- Same as for severe pulmonary blastomycosis, but duration is at least 12 months
- May be followed by lifelong suppressive itraconazole 200 mg po daily if immunosuppression cannot be decreased and they have relapsed despite appropriate therapy
Pregnant women
- Use liposomal amphotericin B 3-5 mg/kg per day
- Avoid azoles for risk of teratogenicity
Children
- Blastomycosis in newborns: amphotericin B deoxycholate 1 mg/kg per day
- Blastomycosis in children
- Mild-to-moderate: itraconazole 10 mg/kg po per day (up to 400 mg) for 6 to 12 months
- Severe blastomycosis: amphotericin B deoxycholate 0.7-1 mg/kg per day or liposomal amphotericin B at 3-5 mg/kg per day, followed by itraconazole 10 mg/kg po per day (up to 400 mg), for a total of 12 months
- Monitor serum levels after 2 weeks
Itraconazole
- Tablet formulation has poorer oral bioavailability than liquid formulation
- Need to avoid PPIs and H2 blockers, as it needs an acidic stomach environment to get absorbed, especially for tablet formulation
- Not as good CNS penetration as other triazoles
- Needs therapeutic drug monitoring after 2 weeks with goal of maintaining serum levels between 1.0 and 10.0 μg/ml
Further Reading
- Chapman SW et al. Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2008 46(12):1801-1812.