Blastomyces dermatitidis
From IDWiki
Blastomyces dermatitidis
Background
Microbiology
- Broad-based dimorphic budding yeast
- Mold at 25-28ºC and yeast at 37ºC
- Branching hyphae 2-3 µm in diameter and right-angle conidiophores resembling lollipops
- Conidia become airborne when disturbed
Epidemiology
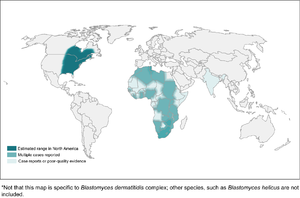
- Present in the Mississippi, Ohio, and St. Lawrence River Valleys, the Great Lakes regions, and western Ontario
- May also be endemic to Africa and India, though it's unclear whether these are true cases or late reactivation
- Hosts include humans, dogs, cats, horses, brown bears, and exotic pets like the kinkajou and red ruffed lemur
- There have been point-source outbreaks associated with occupational and recreational activities, usually along streams or rivers enriched with decaying vegetation
- Possibly has cold-weather seasonality
Pathophysiology
- Inhalation of conidia into the lungs
- Macophages can phagocytize and kill the conidia, and can also slow conversion into yeast form
- A thick cell wall helps to prevent phagocytosis
- Some conidia successfully convert to the pathogenic yeast form
- Major antigens include BAD1 on the cell wall surface and binds CR3 (CD11b/CD18) and CD14
- Humoral immunity has little effect; rather, immune response relies on cell-mediated immunity
Clinical Manifestations
- Can be acute pneumonia (followed by either recovery or chronic infection), or asymptomatic (followed by recovery or chronic infection)
- About 50% overall resolve without treatment
- About half of symptomatic patients have isolated lung involvement and half are disseminated
- When symptomatic, may have non-specific and constitutional symptoms
- Can be primary or reactivation
- Incubation period 3 weeks to 3 months
Respiratory Blastomycosis
- Respiratory symptoms are the most common focus
- Can mimic community-acquired pneumonia or tuberculosis, and may have hemoptysis
- Less likely cavitary, but possible
- Can be acute or chronic presentation, or asymptomatic
- Chronic typically lasts 2 to 6 months, with constitutional symptoms
- Even if there is non-pulmonary infection, there are often findings on chest x-ray
- Can also cause ARDS in about 10% of cases, which distinguishes it from histoplasmosis
Extra-Pulmonary Blastomycosis
- Next most common feature is dissemination to skin
- Lesions usually either verrucous or ulcerative
- May be misdiagnosed as pyoderma gangrenosum, keratoacanthoma, BCC, squamous cell carcinoma, or mycosis fungoides
- Differential also contains NTM, other fungal infections, lupus
- Osteomyelitis, with or without evidence of lung involvement, is the third most common form
- There are no specific clinical or radiographical features of blastomycosis
- Genitourinary involvement, especially prostatitis and epididymo-orchitis, are next most common
- May be cultured in urine collected after prostate massage
- Meningitis and cerebritis/abscess are possible
- Consider screening for it in immunocompromised people
- Cerebellum more common
- CSF culture is insenitive, though PCR is better
- Found in 5-10% of cases of disseminated blasto, but associated with high mortality
- Can have ocular involvement, as well
- Differential would involve bacterial and fungal meningitis/abscess (including cryptococcosis), and Nocardia
- Can also affect larynx, lymphatics or lymph nodes, spleen, and any other organ, though fungemia is rarely found
- Infection can cause endocrinologic abnormalities including adrenal insufficiency, thyroid infection, hypercalcemia (granulomatous)
- There are case reports of diabetes insipidus, and hyperprolactinemia
- Because it can occur in any organ, there are also case reports of breast lesions, tubo-ovarian abscess, otitis media, branchial cleft cyst infection
Pregnancy
- May be higher risk group, and can transmit it to the newborn
Immunocompromised Patients
- Not as commonly described as an opportunistic infection as the other endemic fungi
- Few cases with advanced HIV, but possible
- Sarcoidosis, transplantation, and steroid use are all risk factors
- Infliximab and etanercept are higher risk
Diagnosis
- Requires a microbiologic diagnosis
Microscopy
- Can be directly visualized on exudate, sputum, tissue, or really any sample
- Fairly easy to see with KOH or calcofluor, showing thick-walled, multinucleated, broad-based budding yeast
- Can be seen on histology of skin lesion biopsy with Gomori methenamine silver (GMS) and periodic acid-Schiff (PAS) stains
Culture
- Grows as mycelial (mold) form at 25-30ºC, usually after 1 to 3 weeks, starting as a white mold that slowly turns light brown
- Grows 5-10 days before they develop conidia, so relatively low risk of infection early on
- Usually needs a DNA probe to confirm the species
- Biosafety level 3 pathogen, so needs to be sent to Public Health
Serology
- Antibody
- Complement fixation is insensitive (Sn 9 to 43%); EIA is more sensitive but less specific
- Immunodiffusion is likely better, though sensitivity still rather poor (Sn 28 to 64%, Sp 100%)
- Immunodiffusion for A band is what is done in Ontario
- BAD1 antigen antibodies is 85% sensitive but not yet used
- Urinary antigen has 93% sens and 80% spec
- It cross-reacts with other dimorphic fungi, especially histoplasmosis
- Can be trended to monitor response during therapy
- Can check 1,3-β-d-glucan, but not specific or particularly sensitive
Molecular Methods
- Not yet well-developed, but theoretically possible to do PCR
Management
- Chronic blastomycosis doesn't resolve without treatment, and mortality is as high as 60%
- Although many cases of acute pulmonary blastomycosis self-resolve, it is still recommended to treat, since triazoles are well-tolerated
- Severity is based on clinical judgement, as there are no validated criteria
Pulmonary Blastomycosis
- Mild-to-moderate: itraconazole 200 mg po tid for 3 days followed by bid for 6-12 months
- Moderate severe-to-severe: liposomal amphotericin B 3-5 mg/kg per day for 1-2 weeks or until improvement, followed by itraconazole 200 mg po tid for 3 days, followed by itraconazole 200 mg po bid, for a total of 6 to 12 months
- May need up 6 to 8 weeks of induction with liposomal amphotericin B
- Monitor serum itraconazole after 2 weeks, targeting 1 to 10 μg/mL
Disseminated Extrapulmonary Blastomycosis
- Same as for pulmonary blastomycosis, but treated for at least 12 months if bone involvement
CNS Blastomycosis
- Amphotericin B 5 mg/kg per day for 4-6 weeks followed by an azole for at least 12 months and until resolution of CSF abnormalities
- Azoles include fluconazole 800 mg daily, itraconazole 200 mg bid or tid, or voriconazole 200-300 mg bid
- Voriconazole may be better for CNS disease (better CNS penetration than itraconazole, and very good in vitro activity)
Immunocompromised Patients
- Same as for severe pulmonary blastomycosis, but duration is at least 12 months
- May be followed by lifelong suppressive itraconazole 200 mg po daily if immunosuppression cannot be decreased and they have relapsed despite appropriate therapy
Pregnant women
- Use liposomal amphotericin B 3-5 mg/kg per day
- Avoid azoles for risk of teratogenicity
Children
- Blastomycosis in newborns: amphotericin B deoxycholate 1 mg/kg per day
- Blastomycosis in children
- Mild-to-moderate: itraconazole 10 mg/kg po per day (up to 400 mg) for 6 to 12 months
- Severe blastomycosis: amphotericin B deoxycholate 0.7-1 mg/kg per day or liposomal amphotericin B at 3-5 mg/kg per day, followed by itraconazole 10 mg/kg po per day (up to 400 mg), for a total of 12 months
- Monitor serum levels after 2 weeks
Itraconazole
- Tablet formulation has poorer oral bioavailability than liquid formulation
- Need to avoid PPIs and H2 blockers, as it needs an acidic stomach environment to get absorbed, especially for tablet formulation
- Not as good CNS penetration as other triazoles
- Needs therapeutic drug monitoring after 2 weeks with goal of maintaining serum levels between 1.0 and 10.0 μg/ml
Further Reading
- Chapman SW et al. Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2008 46(12):1801-1812.
References
- a b Nida Ashraf, Ryan C. Kubat, Victoria Poplin, Antoine A. Adenis, David W. Denning, Laura Wright, Orion McCotter, Ilan S. Schwartz, Brendan R. Jackson, Tom Chiller, Nathan C. Bahr. Re-drawing the Maps for Endemic Mycoses. Mycopathologia. 2020;185(5):843-865. doi:10.1007/s11046-020-00431-2.
- ^ Ilan S. Schwartz, Carol A. Kauffman. Blastomycosis. Seminars in Respiratory and Critical Care Medicine. 2020;41(01):031-041. doi:10.1055/s-0039-3400281.
- ^ Laurie A. Proia, Darin O. Harnisch. Successful Use of Posaconazole for Treatment of Blastomycosis. Antimicrobial Agents and Chemotherapy. 2012;56(7):4029-4029. doi:10.1128/aac.00359-12.
- ^ Shandra R. Day, David B. Weiss, Kevin C. Hazen, Christopher C. Moore. Successful treatment of osseous blastomycosis without pulmonary or disseminated disease and review of the literature. Diagnostic Microbiology and Infectious Disease. 2014;79(2):242-244. doi:10.1016/j.diagmicrobio.2014.02.021.
- ^ Johan A Maertens, Galia Rahav, Dong-Gun Lee, Alfredo Ponce-de-León, Isabel Cristina Ramírez Sánchez, Nikolay Klimko, Anne Sonet, Shariq Haider, Juan Diego Vélez, Issam Raad, Liang-Piu Koh, Meinolf Karthaus, Jianying Zhou, Ronen Ben-Ami, Mary R Motyl, Seongah Han, Anjana Grandhi, Hetty Waskin. Posaconazole versus voriconazole for primary treatment of invasive aspergillosis: a phase 3, randomised, controlled, non-inferiority trial. The Lancet. 2021;397(10273):499-509. doi:10.1016/s0140-6736(21)00219-1.
- ^ Oliver A. Cornely, Johan Maertens, Drew J. Winston, John Perfect, Andrew J. Ullmann, Thomas J. Walsh, David Helfgott, Jerzy Holowiecki, Dick Stockelberg, Yeow-Tee Goh, Mario Petrini, Cathy Hardalo, Ramachandran Suresh, David Angulo-Gonzalez. Posaconazole vs. Fluconazole or Itraconazole Prophylaxis in Patients with Neutropenia. New England Journal of Medicine. 2007;356(4):348-359. doi:10.1056/nejmoa061094.
- ^ Michael J Scolarici, Coleton King, Alana Sterkel, Jeannina Smith, Gregory Gauthier, Christopher Saddler. The Role of Isavuconazonium Sulphate for the Treatment of Blastomycosis: A Case Series and Antifungal Susceptibility. Open Forum Infectious Diseases. 2022;9(7). doi:10.1093/ofid/ofac220.
- ^ George R. Thompson, Adrian Rendon, Rodrigo Ribeiro dos Santos, Flavio Queiroz-Telles, Luis Ostrosky-Zeichner, Nkechi Azie, Rochelle Maher, Misun Lee, Laura Kovanda, Marc Engelhardt, Jose A. Vazquez, Oliver A. Cornely, John R. Perfect. Isavuconazole Treatment of Cryptococcosis and Dimorphic Mycoses. Clinical Infectious Diseases. 2016;63(3):356-362. doi:10.1093/cid/ciw305.
- ^ Johan A Maertens, Issam I Raad, Kieren A Marr, Thomas F Patterson, Dimitrios P Kontoyiannis, Oliver A Cornely, Eric J Bow, Galia Rahav, Dionysios Neofytos, Mickael Aoun, John W Baddley, Michael Giladi, Werner J Heinz, Raoul Herbrecht, William Hope, Meinolf Karthaus, Dong-Gun Lee, Olivier Lortholary, Vicki A Morrison, Ilana Oren, Dominik Selleslag, Shmuel Shoham, George R Thompson, Misun Lee, Rochelle M Maher, Anne-Hortense Schmitt-Hoffmann, Bernhardt Zeiher, Andrew J Ullmann. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. The Lancet. 2016;387(10020):760-769. doi:10.1016/s0140-6736(15)01159-9.