Borrelia burgdorferi: Difference between revisions
From IDWiki
Borrelia burgdorferi
Content deleted Content added
m Text replacement - "Clinical Presentation" to "Clinical Manifestations" |
|||
| Line 1: | Line 1: | ||
== |
==Background== |
||
=== |
===Epidemiology=== |
||
====North America==== |
|||
* Transmitted by ''[[Ixodes scapularis]]'' (deer or black-legged tick), or ''[[Ixodes pacificus]]'' in the Pacific US |
|||
* Reservoirs include deer and small mammals such as rodents |
|||
* Lyme species are different outside of North America |
|||
*Transmitted by ''[[Ixodes scapularis]]'' (deer or black-legged tick), or ''[[Ixodes pacificus]]'' in the Pacific US |
|||
=== Europe === |
|||
*Reservoirs include deer and small mammals such as rodents |
|||
* Three species of ''[[Borrelia]]'' exist in Europe |
|||
*Lyme species are different outside of North America |
|||
** ''B. burgdorferi'' |
|||
** ''B. afzelii'' |
|||
** ''B. garinii'' |
|||
* The species have cross-reactivity with Lyme serology |
|||
== |
====Europe==== |
||
*Three main species of ''[[Borrelia]]'' exist in Europe: ''B. burgdorferi'', ''B. afzelii,'' ''B. garinii'' |
|||
*The vectors are [[Ixodes ricinus]] (in Europe and the Near East, and [[Ixodes persulcatus]] in Asia |
|||
*The species have cross-reactivity with Lyme serology |
|||
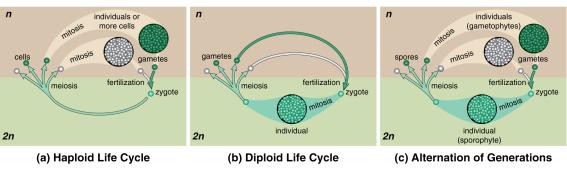
===Life Cycle=== |
|||
[[File:lifecycle.jpg|tick lifecycle]] |
[[File:lifecycle.jpg|tick lifecycle]] |
||
== |
===Pathophysiology=== |
||
* |
*Tick bites host |
||
* |
*''Borrelia'' migrates from hidgut to mouth over ~36 hours, then gets regurgitated into the wound |
||
* |
*Local multiplication followed by dissemination |
||
== |
===Risk Factors=== |
||
* |
*Hiking or camping in Vermont or other endemic area, with known or possible tick exposure |
||
== |
==Clinical Manifestations== |
||
* |
*May not remember tick bite |
||
* |
*There can be overlap between the three stages (early localized, early disseminated, late) |
||
=== |
===Early localized disease (7 days)=== |
||
* |
*Presents within 1 month of exposure |
||
* |
*'''Erythema migrans''' in 80%; appears 7-14 days after tick bite (range 3 to 32 days) |
||
**Expanding red or bluish-red patch ≥5 cm, with or without central clearing |
|||
** If appears immediately and rapidly, think about local irritation and allergy, rather than Lyme |
|||
**Spreads over days |
|||
** Can present atypically, without target appearance, with ulceration, or with vesicles |
|||
**Can present atypically, without target appearance, with ulceration, or with vesicles |
|||
** Spreads 2-3 days daily |
|||
**If appears immediately and rapidly; need to consider local irritation and allergy, rather than Lyme |
|||
* Fever, fatigue, malaise, lethargy |
|||
*Fever, fatigue, malaise, lethargy |
|||
* Mild headache and neck stiffness |
|||
* |
*Mild headache and neck stiffness |
||
*Myalgias and arthralgias |
|||
* May have mildly elevated liver enzymes |
|||
*May have mildly elevated liver enzymes |
|||
=== |
===Early disseminated disease (14-21 days)=== |
||
* |
*Early disseminated (weeks to months), inflammatory phase |
||
* |
*Can be a non-specific febrile illness with headaches, arthralgias and fatigue, but can also cause a number of other symptoms |
||
* |
**[[Bell palsy]], unilateral or bilateral, or other cranial nerve palsies |
||
**[[Aseptic meningitis]] with lymphocytosis |
|||
* Multiple rashes |
|||
**[[Carditis]] with [[heart block]] |
|||
* Cranial nerve palsies, lymphocytic meningitis, conjunctivitis, arthralgia, myalgia, headache, fatigue, carditis (heart block) |
|||
**Secondary skin lesions |
|||
**[[Conjunctivitis]] |
|||
=== |
===Neuroborreliosis=== |
||
*Refers specifically to the neurological manifestations of early disseminated Lyme disease |
|||
* Meningo-radiculitis, meningitis, and peripheral facial palsy |
|||
*More common with [[Borrelia garinii]] |
|||
* CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
|||
*[[Meningo-radiculitis]], [[meningitis]], and peripheral [[facial nerve palsy]] |
|||
*Rarely, [[encephalitis]] or [[myelitis]] or [[cerebral vasculitis]] |
|||
*CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
|||
=== |
===Cardiac Lyme=== |
||
* |
*AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation |
||
* |
*Resolves with treatment, so only ever needs temporary pacemaker |
||
=== |
===Late disease=== |
||
* |
*Late or chronic (months to years), less inflammatory, usually within a single body site |
||
* |
*Arthritis in 60% of untreated patients, now down to 15-20% |
||
** |
**PCR of synovial fluid |
||
* |
*Encephalomyelitis/encephalopathy next-most common |
||
** |
**LP fairly benign, with slightly elevated protein |
||
** |
**Diagnose with simultaneous serum/CSF antibodies |
||
* |
*Peripheral neuropathy |
||
* |
*Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue |
||
=== |
===Lyme arthritis=== |
||
* |
*Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation |
||
* |
*Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs |
||
=== |
===Acrodermatitis chronica artophicans=== |
||
* |
*Chronic red or bluish-red leions, usually on the extensor surgaces |
||
* |
*Initially doughy, eventually atrophic |
||
* |
*Can occur up to 8 years after infection |
||
=== |
===Late neuroborereliosis=== |
||
* |
*Encephalopathy, encephalitis, and peripheral neuropathy |
||
=== |
===Complications=== |
||
* |
*Carditis in 5% of untreated patients |
||
** |
**Heart block |
||
** |
**Cardiomyopathy |
||
* |
*Neurologic involvement in 15% of untreated patients |
||
** |
**Uni- or bilateral cranial nerve defects, especially '''CN VII''' |
||
** |
**Meningitis and encephalitis |
||
* |
*Migratory arthralgias in 60% of untreated patients |
||
* |
*Conjunctivitis in 10% of untreated patients |
||
* |
*Regional or generalized lymphadenopathy |
||
=== |
===Borrelial lymphocytoma=== |
||
* |
*Painless bluish-red nodule, usually on the ear, nipple, or scrotum |
||
* |
*More common in adults |
||
=== |
===Ocular manifestations=== |
||
* |
*Conjunctivitis, uveitis, papillitis, episcleritis, keratitis |
||
=== |
===Coinfection=== |
||
*Can have thrombocytopenia and anemia if coinfected with ''Anaplasma'' or ''Babesia'' |
|||
===Post-Lyme disease syndrome=== |
|||
*Subjective symptoms that persist following treatment, without objective clinical findings of infection |
|||
== Differential Diagnosis == |
|||
=== Erythema Migrans === |
|||
* Tick or insect bite hypersensitivity reaction |
|||
* [[Cellulitis]], [[erysipelas]] |
|||
* [[Erythema multiforme]] |
|||
* [[STARI]] |
|||
* [[Tinea]] |
|||
* [[Nummular eczema]] |
|||
* [[Granuloma annulare]] |
|||
* [[Contact dermatitis]] |
|||
* [[Urticaria]] |
|||
* [[Fixed drug eruption]] |
|||
* [[Pityriasis rosea]] |
|||
* [[Parvovirus B19]] (in children) |
|||
=== Borrelial Lymphocytoma === |
|||
* [[Breast cancer]] |
|||
* [[B-cell lymphoma]] |
|||
* [[Pseudolymphoma]] |
|||
=== Lyme neuroborreliosis === |
|||
* Other causes of [[facial nerve palsy]] |
|||
* [[Viral meningitis]] |
|||
* [[Mechanical radiculopathy]] |
|||
* First episode of relapsin-remitting [[multiple sclerosis]] |
|||
* Primary progressive [[multiple sclerosis]] |
|||
=== Lyme carditis === |
|||
* Other causes of [[heart block]] or [[myopericarditis]] |
|||
=== Lyme arthritis === |
|||
* [[Gout]] or [[pseudogout]] |
|||
* Can have thrombocytopenia and anemia if coinfected with ''Anaplasma'' or ''Babesia'' |
|||
* [[Septic arthritis]] |
|||
* [[Viral arthritis]] |
|||
* [[Psoriatic arthritis]] |
|||
* [[Juvenile oligoarthritis]] |
|||
* [[Reactive arthritis]] |
|||
* [[Sarcoidosis]] |
|||
* Early [[rheumatoid arthritis]] |
|||
* [[Seronegative spondyloarthropathies]] |
|||
=== |
=== Acrodermatitis Chronic Atrophicans === |
||
* Old age |
|||
* Subjective symptoms that persist following treatment, without objective clinical findings of infection |
|||
* Chillblains |
|||
* Chronic venous insufficiency |
|||
* Superficial [[thrombophlebitis]] |
|||
* Hypostatic [[eczema]] |
|||
* Arterial obliterative disease |
|||
* [[Acrocyanosis]] |
|||
* [[Livedo reticularis]] |
|||
* [[Lymphoedema]] |
|||
* [[Erythromelalgia]] |
|||
* [[Scleroderma]] |
|||
* Rheumatoid nodules |
|||
* Gouty tophi |
|||
* [[Erythema nodosum]] |
|||
== |
==Diagnosis== |
||
* |
*Treatment should be based on symptoms and compatible exposure history |
||
** |
**If EM present, further testing is unhelpful outside of unusual cases |
||
* |
*Usually done by serology, with EIA followed by reflexive Western blot |
||
** |
**EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely |
||
*** |
***Usually positive around 2 weeks |
||
*** |
***False negatives common early in clinical course |
||
*** |
***False positives with HIV, hepatitis C, and syphilis |
||
*** |
***Cross-reacts with European Lyme |
||
** |
**Western blot split into IgM and IgG if positive or equivocal |
||
*** |
***IgM 4 weeks, IgG 8 weeks |
||
*** |
***IgM is prone to over-interpretation and false positives |
||
*** |
***Does NOT cross-react with European Lyme (in Ontario) |
||
** |
**Serology is most helpful when the pretest probability is >20% |
||
* |
*CSF antibodies is useful for neuroborreliosis, but persist years after treatment |
||
* |
*PCR may be helpful in cases where patients are from populations with high seroprevalence |
||
** |
**Pretty good for joint, less sensitive for CSF |
||
=== |
===Lyme Serology=== |
||
{| class="wikitable" |
{| class="wikitable" |
||
! |
!EIA |
||
! |
!Western blot |
||
! |
!Interpretation |
||
! |
!Action |
||
|- |
|- |
||
| + |
| + |
||
| + |
| + |
||
| |
|Early disseminated or late disease<br />Previous exposure, treated or not |
||
| |
|Treat if compatible symptoms and history |
||
|- |
|- |
||
| + |
| + |
||
| |
|– |
||
| |
|Early disease<br />Early disease, treated<br />European Lyme<br />False-positive |
||
| |
|If <8 weeks from exposure, repeat<br />If >8 weeks, look for other cause<br />Rule out HIV, hepatitis C, and syphilis<br />Assess for autoimmune diseases<br />Consider European Lyme |
||
|- |
|- |
||
| |
|– |
||
| |
|– |
||
| |
|Very early Lyme <2 weeks<br />Negative |
||
| |
|Treat if erythema migrans |
||
|} |
|} |
||
== |
==Management== |
||
* |
*[[Doxycycline]] 100mg po BID x14 days |
||
** |
**7 to 21 days, depending on severity |
||
* |
*Alternative: [[amoxicillin]] 500mg po TID or [[cefuroxime]] 500mg po BID or [[azithromycin]] |
||
* |
*Parenteral antibiotics for CNS or cardiac disease |
||
== |
==Further Reading== |
||
* |
*Health Quality Ontario (2018). [https://www.hqontario.ca/Evidence-to-Improve-Care/Evidence-and-Health-Quality-Ontario/Guidance-Documents Management of Tick Bites and Investigation of Early Localized Lyme Disease]. |
||
{{DISPLAYTITLE:''Borrelia burgdorferi''}} |
{{DISPLAYTITLE:''Borrelia burgdorferi''}} |
||
Revision as of 17:51, 17 August 2020
Background
Epidemiology
North America
- Transmitted by Ixodes scapularis (deer or black-legged tick), or Ixodes pacificus in the Pacific US
- Reservoirs include deer and small mammals such as rodents
- Lyme species are different outside of North America
Europe
- Three main species of Borrelia exist in Europe: B. burgdorferi, B. afzelii, B. garinii
- The vectors are Ixodes ricinus (in Europe and the Near East, and Ixodes persulcatus in Asia
- The species have cross-reactivity with Lyme serology
Life Cycle
Pathophysiology
- Tick bites host
- Borrelia migrates from hidgut to mouth over ~36 hours, then gets regurgitated into the wound
- Local multiplication followed by dissemination
Risk Factors
- Hiking or camping in Vermont or other endemic area, with known or possible tick exposure
Clinical Manifestations
- May not remember tick bite
- There can be overlap between the three stages (early localized, early disseminated, late)
Early localized disease (7 days)
- Presents within 1 month of exposure
- Erythema migrans in 80%; appears 7-14 days after tick bite (range 3 to 32 days)
- Expanding red or bluish-red patch ≥5 cm, with or without central clearing
- Spreads over days
- Can present atypically, without target appearance, with ulceration, or with vesicles
- If appears immediately and rapidly; need to consider local irritation and allergy, rather than Lyme
- Fever, fatigue, malaise, lethargy
- Mild headache and neck stiffness
- Myalgias and arthralgias
- May have mildly elevated liver enzymes
Early disseminated disease (14-21 days)
- Early disseminated (weeks to months), inflammatory phase
- Can be a non-specific febrile illness with headaches, arthralgias and fatigue, but can also cause a number of other symptoms
- Bell palsy, unilateral or bilateral, or other cranial nerve palsies
- Aseptic meningitis with lymphocytosis
- Carditis with heart block
- Secondary skin lesions
- Conjunctivitis
Neuroborreliosis
- Refers specifically to the neurological manifestations of early disseminated Lyme disease
- More common with Borrelia garinii
- Meningo-radiculitis, meningitis, and peripheral facial nerve palsy
- Rarely, encephalitis or myelitis or cerebral vasculitis
- CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose
Cardiac Lyme
- AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation
- Resolves with treatment, so only ever needs temporary pacemaker
Late disease
- Late or chronic (months to years), less inflammatory, usually within a single body site
- Arthritis in 60% of untreated patients, now down to 15-20%
- PCR of synovial fluid
- Encephalomyelitis/encephalopathy next-most common
- LP fairly benign, with slightly elevated protein
- Diagnose with simultaneous serum/CSF antibodies
- Peripheral neuropathy
- Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue
Lyme arthritis
- Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation
- Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs
Acrodermatitis chronica artophicans
- Chronic red or bluish-red leions, usually on the extensor surgaces
- Initially doughy, eventually atrophic
- Can occur up to 8 years after infection
Late neuroborereliosis
- Encephalopathy, encephalitis, and peripheral neuropathy
Complications
- Carditis in 5% of untreated patients
- Heart block
- Cardiomyopathy
- Neurologic involvement in 15% of untreated patients
- Uni- or bilateral cranial nerve defects, especially CN VII
- Meningitis and encephalitis
- Migratory arthralgias in 60% of untreated patients
- Conjunctivitis in 10% of untreated patients
- Regional or generalized lymphadenopathy
Borrelial lymphocytoma
- Painless bluish-red nodule, usually on the ear, nipple, or scrotum
- More common in adults
Ocular manifestations
- Conjunctivitis, uveitis, papillitis, episcleritis, keratitis
Coinfection
- Can have thrombocytopenia and anemia if coinfected with Anaplasma or Babesia
Post-Lyme disease syndrome
- Subjective symptoms that persist following treatment, without objective clinical findings of infection
Differential Diagnosis
Erythema Migrans
- Tick or insect bite hypersensitivity reaction
- Cellulitis, erysipelas
- Erythema multiforme
- STARI
- Tinea
- Nummular eczema
- Granuloma annulare
- Contact dermatitis
- Urticaria
- Fixed drug eruption
- Pityriasis rosea
- Parvovirus B19 (in children)
Borrelial Lymphocytoma
Lyme neuroborreliosis
- Other causes of facial nerve palsy
- Viral meningitis
- Mechanical radiculopathy
- First episode of relapsin-remitting multiple sclerosis
- Primary progressive multiple sclerosis
Lyme carditis
- Other causes of heart block or myopericarditis
Lyme arthritis
- Gout or pseudogout
- Septic arthritis
- Viral arthritis
- Psoriatic arthritis
- Juvenile oligoarthritis
- Reactive arthritis
- Sarcoidosis
- Early rheumatoid arthritis
- Seronegative spondyloarthropathies
Acrodermatitis Chronic Atrophicans
- Old age
- Chillblains
- Chronic venous insufficiency
- Superficial thrombophlebitis
- Hypostatic eczema
- Arterial obliterative disease
- Acrocyanosis
- Livedo reticularis
- Lymphoedema
- Erythromelalgia
- Scleroderma
- Rheumatoid nodules
- Gouty tophi
- Erythema nodosum
Diagnosis
- Treatment should be based on symptoms and compatible exposure history
- If EM present, further testing is unhelpful outside of unusual cases
- Usually done by serology, with EIA followed by reflexive Western blot
- EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely
- Usually positive around 2 weeks
- False negatives common early in clinical course
- False positives with HIV, hepatitis C, and syphilis
- Cross-reacts with European Lyme
- Western blot split into IgM and IgG if positive or equivocal
- IgM 4 weeks, IgG 8 weeks
- IgM is prone to over-interpretation and false positives
- Does NOT cross-react with European Lyme (in Ontario)
- Serology is most helpful when the pretest probability is >20%
- EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely
- CSF antibodies is useful for neuroborreliosis, but persist years after treatment
- PCR may be helpful in cases where patients are from populations with high seroprevalence
- Pretty good for joint, less sensitive for CSF
Lyme Serology
| EIA | Western blot | Interpretation | Action |
|---|---|---|---|
| + | + | Early disseminated or late disease Previous exposure, treated or not |
Treat if compatible symptoms and history |
| + | – | Early disease Early disease, treated European Lyme False-positive |
If <8 weeks from exposure, repeat If >8 weeks, look for other cause Rule out HIV, hepatitis C, and syphilis Assess for autoimmune diseases Consider European Lyme |
| – | – | Very early Lyme <2 weeks Negative |
Treat if erythema migrans |
Management
- Doxycycline 100mg po BID x14 days
- 7 to 21 days, depending on severity
- Alternative: amoxicillin 500mg po TID or cefuroxime 500mg po BID or azithromycin
- Parenteral antibiotics for CNS or cardiac disease
Further Reading
- Health Quality Ontario (2018). Management of Tick Bites and Investigation of Early Localized Lyme Disease.