Borrelia burgdorferi: Difference between revisions
From IDWiki
Borrelia burgdorferi
Content deleted Content added
Imported from text file |
No edit summary |
||
| (23 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
==Background== |
|||
= Lyme disease (''Borrelia burgdorferi'') = |
|||
== |
=== Microbiology === |
||
* Spirochete |
|||
* Transmitted by ''Ixodes scapularis'' (deer or black-legged tick), or ''I. pacificus'' in the Pacific US |
|||
* Lyme disease can also be caused by [[Borrelia mayonii]] |
|||
* Reservoirs include deer and small mammals such as rodents |
|||
* Lyme species are different outside of North America |
|||
===Epidemiology=== |
|||
 |
|||
*Most cases occur during June and July, when nymphal ticks are most active and people are outdoors |
|||
[[File:image-20190117091839996.png|image-20190117091839996]] |
|||
*Infection is possible year-round, though, with ticks being active any time temperatures are above freezing |
|||
=== |
====North America==== |
||
*Transmitted by ''[[Ixodes scapularis]]'' (deer or black-legged tick), or ''[[Ixodes pacificus]]'' in the Pacific US |
|||
* Three species of ''Borrelia'' exist in Europe, including ''B. burgdorferi'', though the species have cross-reactivity with Lyme serology |
|||
*Reservoirs include deer and small mammals such as rodents |
|||
** ''B. afzelii'' and ''B. garinii'' |
|||
*Lyme species are different outside of North America |
|||
== |
====Europe==== |
||
*Three main species of ''[[Borrelia]]'' exist in Europe: ''B. burgdorferi'', ''B. afzelii,'' ''B. garinii'' |
|||
*The vectors are [[Ixodes ricinus]] (in Europe and the Near East, and [[Ixodes persulcatus]] in Asia |
|||
*The species have cross-reactivity with Lyme serology |
|||
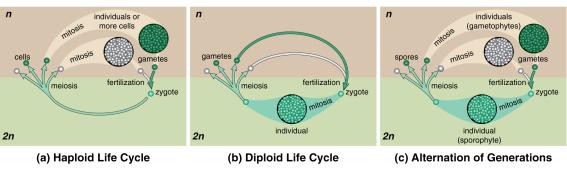
===Life Cycle=== |
|||
[[File:lifecycle.jpg|tick lifecycle]] |
[[File:lifecycle.jpg|tick lifecycle]] |
||
== |
===Pathophysiology=== |
||
* |
*Tick bites host |
||
* |
*''Borrelia'' migrates from hindgut to mouth over ~36 hours, then gets regurgitated into the wound |
||
**May take as little as 24 hours |
|||
* Local multiplication followed by dissemination |
|||
*Local multiplication followed by dissemination |
|||
== |
===Risk Factors=== |
||
* |
*Hiking or camping in Vermont or other endemic area, with known or possible tick exposure |
||
== |
==Clinical Manifestations== |
||
* |
*May not remember tick bite |
||
* |
*There can be overlap between the three stages (early localized, early disseminated, late) |
||
*Requires minimum of 24 hours of tick attachment, but typically takes 36 hours or longer |
|||
=== |
===Early Localized Disease (7 days)=== |
||
* |
*Presents within 1 month of exposure |
||
* |
*'''Erythema migrans''' in 80%; appears 7-14 days after tick bite (range 3 to 32 days) |
||
**Expanding red or bluish-red patch ≥5 cm, with or without central clearing |
|||
** If appears immediately and rapidly, think about local irritation and allergy, rather than Lyme |
|||
**Spreads over days |
|||
** Can present atypically, without target appearance, with ulceration, or with vesicles |
|||
**Can present atypically, without target appearance, with ulceration, or with vesicles |
|||
** Spreads 2-3 days daily |
|||
**If appears immediately and rapidly; need to consider local irritation and allergy, rather than Lyme |
|||
* Fever, fatigue, malaise, lethargy |
|||
*Fever, fatigue, malaise, lethargy |
|||
* Mild headache and neck stiffness |
|||
* |
*Mild headache and neck stiffness |
||
*Myalgias and arthralgias |
|||
* May have mildly elevated liver enzymes |
|||
*May have mildly elevated liver enzymes |
|||
=== |
===Early Disseminated Disease (14-21 days)=== |
||
* |
*Early disseminated (weeks to months), inflammatory phase |
||
* |
*Can be a non-specific febrile illness with headaches, arthralgias and fatigue, but can also cause a number of other symptoms |
||
* |
**[[Bell palsy]], unilateral or bilateral, or other cranial nerve palsies |
||
**[[Aseptic meningitis]] with lymphocytosis |
|||
* Multiple rashes |
|||
**[[Carditis]] with [[heart block]] |
|||
* Cranial nerve palsies, lymphocytic meningitis, conjunctivitis, arthralgia, myalgia, headache, fatigue, carditis (heart block) |
|||
**Secondary skin lesions |
|||
**[[Conjunctivitis]] |
|||
==== |
====Neuroborreliosis==== |
||
*Refers specifically to the neurological manifestations of early disseminated Lyme disease |
|||
* Meningo-radiculitis, meningitis, and peripheral facial palsy |
|||
*More common with [[Borrelia garinii]] |
|||
* CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
|||
*[[Meningo-radiculitis]], [[meningitis]], and peripheral [[facial nerve palsy]] |
|||
*Rarely, [[encephalitis]] or [[myelitis]] or [[cerebral vasculitis]] |
|||
*CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
|||
==== |
====Cardiac Lyme==== |
||
* |
*AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation |
||
* |
*Resolves with treatment, so only ever needs temporary pacemaker |
||
=== |
===Late Disease=== |
||
* |
*Late or chronic (months to years), less inflammatory, usually within a single body site |
||
* |
*Arthritis in 60% of untreated patients, now down to 15-20% |
||
** |
**PCR of synovial fluid |
||
* |
*Encephalomyelitis/encephalopathy next-most common |
||
** |
**LP fairly benign, with slightly elevated protein |
||
** |
**Diagnose with simultaneous serum/CSF antibodies |
||
* |
*Peripheral neuropathy |
||
* |
*Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue |
||
==== |
====Lyme Arthritis==== |
||
* |
*Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation |
||
* |
*Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs |
||
==== |
====Acrodermatitis Chronica Atrophicans==== |
||
* |
*Chronic red or bluish-red leions, usually on the extensor surgaces |
||
* |
*Initially doughy, eventually atrophic |
||
* |
*Can occur up to 8 years after infection |
||
==== |
====Late Neuroborreliosis==== |
||
* |
*Encephalopathy, encephalitis, and peripheral neuropathy |
||
=== |
===Complications=== |
||
* |
*Carditis in 5% of untreated patients |
||
** |
**Heart block |
||
** |
**Cardiomyopathy |
||
* |
*Neurologic involvement in 15% of untreated patients |
||
** |
**Uni- or bilateral cranial nerve defects, especially '''CN VII''' |
||
** |
**Meningitis and encephalitis |
||
* |
*Migratory arthralgias in 60% of untreated patients |
||
* |
*Conjunctivitis in 10% of untreated patients |
||
* |
*Regional or generalized lymphadenopathy |
||
=== |
====Borrelial Lymphocytoma==== |
||
* |
*Painless bluish-red nodule, usually on the ear, nipple, or scrotum |
||
* |
*More common in adults |
||
=== |
====Ocular Manifestations==== |
||
* |
*Conjunctivitis, uveitis, papillitis, episcleritis, keratitis |
||
=== |
===Coinfections=== |
||
*''[[Anaplasma]]'' or ''[[Babesia]]'' may be transmitted by the same ticks in areas of endemicity |
|||
* Can have thrombocytopenia and anemia if coinfected with ''Anaplasma'' or ''Babesia'' |
|||
*Can have [[thrombocytopenia]], [[leukopenia]], [[neutropenia]], and [[anemia]] |
|||
**Hemolytic anemia is highly suggestive of [[Babesia microti]] |
|||
*Other signs include fever lasting more than one day after start of antibiotics, especially for [[Babesia microti]] |
|||
=== |
===Post-Lyme Disease Syndrome=== |
||
* |
*Subjective symptoms that persist following treatment, without objective clinical findings of infection |
||
== Diagnosis |
==Differential Diagnosis== |
||
===Erythema Migrans=== |
|||
* Treatment should be based on symptoms and compatible exposure history |
|||
** If EM present, further testing is unhelpful outside of unusual cases |
|||
* Usually done by serology, with EIA followed by reflexive Western blot |
|||
** EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely |
|||
*** Usually positive around 2 weeks |
|||
*** False negatives common early in clinical course |
|||
*** False positives with HIV, hepatitis C, and syphilis |
|||
*** Cross-reacts with European Lyme |
|||
** Western blot split into IgM and IgG if positive or equivocal |
|||
*** IgM 4 weeks, IgG 8 weeks |
|||
*** IgM is prone to over-interpretation and false positives |
|||
*** Does NOT cross-react with European Lyme (in Ontario) |
|||
** Serology is most helpful when the pretest probability is >20% |
|||
* CSF antibodies is useful for neuroborreliosis, but persist years after treatment |
|||
* PCR may be helpful in cases where patients are from populations with high seroprevalence |
|||
** Pretty good for joint, less sensitive for CSF |
|||
*Tick or insect bite hypersensitivity reaction |
|||
=== Lyme Serology === |
|||
*[[Cellulitis]], [[erysipelas]] |
|||
*[[Erythema multiforme]] |
|||
*[[STARI]] |
|||
*[[Tinea]] |
|||
*[[Nummular eczema]] |
|||
*[[Granuloma annulare]] |
|||
*[[Contact dermatitis]] |
|||
*[[Urticaria]] |
|||
*[[Fixed drug eruption]] |
|||
*[[Pityriasis rosea]] |
|||
*[[Parvovirus B19]] (in children) |
|||
===Borrelial Lymphocytoma=== |
|||
{| |
|||
! EIA |
|||
*[[Breast cancer]] |
|||
! Western blot |
|||
*[[B-cell lymphoma]] |
|||
! Interpretation |
|||
*[[Pseudolymphoma]] |
|||
! Action |
|||
===Lyme Neuroborreliosis=== |
|||
*Other causes of [[facial nerve palsy]] |
|||
*[[Viral meningitis]] |
|||
*[[Mechanical radiculopathy]] |
|||
*First episode of relapsin-remitting [[multiple sclerosis]] |
|||
*Primary progressive [[multiple sclerosis]] |
|||
===Lyme Carditis=== |
|||
*Other causes of [[heart block]] or [[myopericarditis]] |
|||
===Lyme Arthritis=== |
|||
*[[Gout]] or [[pseudogout]] |
|||
*[[Septic arthritis]] |
|||
*[[Viral arthritis]] |
|||
*[[Psoriatic arthritis]] |
|||
*[[Juvenile oligoarthritis]] |
|||
*[[Reactive arthritis]] |
|||
*[[Sarcoidosis]] |
|||
*Early [[rheumatoid arthritis]] |
|||
*[[Seronegative spondyloarthropathies]] |
|||
===Acrodermatitis Chronic Atrophicans=== |
|||
*Old age |
|||
*Chillblains |
|||
*Chronic venous insufficiency |
|||
*Superficial [[thrombophlebitis]] |
|||
*Hypostatic [[eczema]] |
|||
*Arterial obliterative disease |
|||
*[[Acrocyanosis]] |
|||
*[[Livedo reticularis]] |
|||
*[[Lymphoedema]] |
|||
*[[Erythromelalgia]] |
|||
*[[Scleroderma]] |
|||
*Rheumatoid nodules |
|||
*Gouty tophi |
|||
*[[Erythema nodosum]] |
|||
==Diagnosis== |
|||
*Treatment should be based on symptoms and compatible exposure history |
|||
**If erythema migrans is present, further testing is unhelpful outside of unusual cases and is not routinely recommended |
|||
*The most commonly used test is serology from blood, with EIA followed by reflexive Western blot |
|||
*CSF antibodies is useful for neuroborreliosis, but persist years after treatment |
|||
*PCR may be helpful in cases where patients are from populations with high seroprevalence |
|||
**Pretty good for joint, less sensitive for CSF |
|||
===Lyme Serology=== |
|||
* Typically done as a screening EIA followed by reflexive Western blot |
|||
** In Ontario, the screening test is Borrelia Vls1/pepC10 IgM/IgG ELISA |
|||
** The Western blot is done for IgM and IgG |
|||
* EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely |
|||
**Usually positive around 2 weeks |
|||
**False negatives common early in clinical course |
|||
**False positives with [[HIV]], [[hepatitis C]], and [[syphilis]] |
|||
**Cross-reacts with European Lyme |
|||
*Western blot split into IgM and IgG if positive or equivocal |
|||
**IgM 4 weeks, IgG 8 weeks |
|||
**IgM is prone to over-interpretation and false positives |
|||
***False positives with [[spirochetes]] ([[syphilis]]), viruses ([[cytomegalovirus]], [[Epstein-Barr virus]], [[hepatitis B virus]], [[hepatitis C virus]], and [[parvovirus B19]]), and bacteria |
|||
**Does NOT cross-react with European Lyme (in Ontario) |
|||
*Serology is most helpful when the pretest probability is >20% |
|||
*Serology remains elevated to months to years and should not be used to monitor response to treatment |
|||
{| class="wikitable" |
|||
!EIA |
|||
!Western Blot |
|||
!Interpretation |
|||
!Action |
|||
|- |
|- |
||
| + |
| + |
||
| + |
| + |
||
| |
|Early disseminated or late disease<br />Previous exposure, treated or not |
||
| |
|Treat if compatible symptoms and history |
||
|- |
|- |
||
| + |
| + |
||
| |
|– |
||
| |
|Early disease<br />Early disease, treated<br />European Lyme<br />False-positive |
||
| |
|If <8 weeks from exposure, repeat<br />If >8 weeks, look for other cause<br />Rule out [[HIV]], [[hepatitis C]], and [[syphilis]]<br />Assess for autoimmune diseases<br />Consider European Lyme |
||
|- |
|- |
||
| |
|– |
||
| |
|– |
||
| |
|Very early Lyme <2 weeks<br />Negative |
||
| |
|Treat if [[erythema migrans]] |
||
|} |
|} |
||
* Health Canada now recommends a modified two-tier EIA with combined IgM/IgG, with the screening EIA done with whole-cell lysate and the confirmatory EIA done with a recombinant protein |
|||
== Management == |
|||
** This approach has increased sensitivity at all stages (50-60% for early Lyme, around 100% for late Lyme including Lyme arthritis), and maintains |
|||
** If you get a negative result when there is high pre-test probability for early Lyme, then submit a follow-up serology 3 to 6 weeks later |
|||
{| class="wikitable" |
|||
!EIA 1 |
|||
!EIA 2 |
|||
!Interpretation |
|||
|- |
|||
|– |
|||
|N/A |
|||
|Negative; consider alternative diagnosis or resubmit in 3-6 weeks if compatible with early Lyme |
|||
|- |
|||
| +/± |
|||
| +/± |
|||
|Positive; treat based on clinical syndrome, if appropriate |
|||
|- |
|||
| +/± |
|||
|– |
|||
|Negative; consider alternative diagnosis or resubmit in 3-6 weeks if compatible with early Lyme |
|||
|} |
|||
==Management== |
|||
===Erythema Migrans=== |
|||
*[[Doxycycline]] 100 mg PO bid for 10 days |
|||
*Second-line: [[amoxicillin]] 500 mg PO tid for 14 days, [[cefuroxime]] 500 mg PO bid for 14 days |
|||
*Third-line: [[azithromycin]] for 7 days |
|||
===Neurological Lyme Disease=== |
|||
*Any of the following: [[ceftriaxone]] IV, [[cefotaxime]] IV, [[penicillin G]] IV, [[doxycycline]] PO |
|||
*Duration of 14 to 21 days |
|||
*If there is parenchymal involvement, which is rare and usually based on MRI |
|||
**If present, prefer IV antibiotics and a 2 to 4 week course |
|||
*In cases of facial nerve palsy, they may also receive [[corticosteroids]] within 72 hours |
|||
===Lyme Carditis=== |
|||
*See [[Lyme carditis#Management|Lyme carditis]] |
|||
===Lyme Arthritis=== |
|||
*Oral antibiotics for 28 days |
|||
*If no response to oral antibiotics, can consider a course of [[ceftriaxone]] IV for 2 to 4 weeks |
|||
===Post-Antibiotic Lyme Arthritis=== |
|||
*Refer to rheumatologist for consideration of DMARDs, biologics, intraarticular steroid injections, or arthroscopic synovectomy |
|||
===Borrelial Lymphocytoma=== |
|||
*Oral antibiotics for 14 days |
|||
===Acrodermatitis Chronica Atrophicans=== |
|||
*Oral antibiotics for 21 to 28 days |
|||
==Prevention== |
|||
*Routine personal protective measures to reduce tick exposure |
|||
*DEET, picaridin, IR3535, oil of lemon eucalyptus, PMD, 2-undecanone, or permethrin |
|||
*Remove ticks with clean fine-tipped tweezer inserted between the tick body and the skin |
|||
**Do not cover, spray, or burn the tick |
|||
**See [[tick removal]] for more information |
|||
===Prophylaxis=== |
|||
*Can be considered in children and adults within 72 hours of tick removal if all of the following criteria are met: |
|||
**[[Ixodes]] tick is identified |
|||
***Small, tear-drop shaped |
|||
***Plain oval shield |
|||
***Lack of festoons |
|||
**Occurs in a highly endemic area |
|||
**Tick was attached for ≥36 hours |
|||
***You can get a sense by asking if the tick was flat or engorged |
|||
***If definitely flat, almost certainly attached less than 36 hours |
|||
***However, still looks flat at 24 hours |
|||
*Use a single oral dose of [[doxycycline]] 4.4 mg/kg (max 200 mg) for children or 200 mg for adults |
|||
==Further Reading== |
|||
* Doxycycline 100mg po BID x14 days |
|||
** 7 to 21 days, depending on severity |
|||
* Alternative: amoxicillin 500mg po TID or cefuroxime 500mg po BID or azithromycin |
|||
* Parenteral antibiotics for CNS or cardiac disease |
|||
*2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. ''Clin Infect Dis''. 2020. doi: [https://doi.org/10.1093/cid/ciaa1215 10.1093/cid/ciaa1215] |
|||
== Further Reading == |
|||
*Health Quality Ontario (2018). [https://www.hqontario.ca/Evidence-to-Improve-Care/Evidence-and-Health-Quality-Ontario/Guidance-Documents Management of Tick Bites and Investigation of Early Localized Lyme Disease]. |
|||
{{DISPLAYTITLE:''Borrelia burgdorferi''}} |
|||
* Health Quality Ontario (2018). [https://www.hqontario.ca/Evidence-to-Improve-Care/Evidence-and-Health-Quality-Ontario/Guidance-Documents Management of Tick Bites and Investigation of Early Localized Lyme Disease]. |
|||
[[Category:Borrelioses]] |
|||
Latest revision as of 13:32, 2 August 2024
Background
Microbiology
- Spirochete
- Lyme disease can also be caused by Borrelia mayonii
Epidemiology
- Most cases occur during June and July, when nymphal ticks are most active and people are outdoors
- Infection is possible year-round, though, with ticks being active any time temperatures are above freezing
North America
- Transmitted by Ixodes scapularis (deer or black-legged tick), or Ixodes pacificus in the Pacific US
- Reservoirs include deer and small mammals such as rodents
- Lyme species are different outside of North America
Europe
- Three main species of Borrelia exist in Europe: B. burgdorferi, B. afzelii, B. garinii
- The vectors are Ixodes ricinus (in Europe and the Near East, and Ixodes persulcatus in Asia
- The species have cross-reactivity with Lyme serology
Life Cycle
Pathophysiology
- Tick bites host
- Borrelia migrates from hindgut to mouth over ~36 hours, then gets regurgitated into the wound
- May take as little as 24 hours
- Local multiplication followed by dissemination
Risk Factors
- Hiking or camping in Vermont or other endemic area, with known or possible tick exposure
Clinical Manifestations
- May not remember tick bite
- There can be overlap between the three stages (early localized, early disseminated, late)
- Requires minimum of 24 hours of tick attachment, but typically takes 36 hours or longer
Early Localized Disease (7 days)
- Presents within 1 month of exposure
- Erythema migrans in 80%; appears 7-14 days after tick bite (range 3 to 32 days)
- Expanding red or bluish-red patch ≥5 cm, with or without central clearing
- Spreads over days
- Can present atypically, without target appearance, with ulceration, or with vesicles
- If appears immediately and rapidly; need to consider local irritation and allergy, rather than Lyme
- Fever, fatigue, malaise, lethargy
- Mild headache and neck stiffness
- Myalgias and arthralgias
- May have mildly elevated liver enzymes
Early Disseminated Disease (14-21 days)
- Early disseminated (weeks to months), inflammatory phase
- Can be a non-specific febrile illness with headaches, arthralgias and fatigue, but can also cause a number of other symptoms
- Bell palsy, unilateral or bilateral, or other cranial nerve palsies
- Aseptic meningitis with lymphocytosis
- Carditis with heart block
- Secondary skin lesions
- Conjunctivitis
Neuroborreliosis
- Refers specifically to the neurological manifestations of early disseminated Lyme disease
- More common with Borrelia garinii
- Meningo-radiculitis, meningitis, and peripheral facial nerve palsy
- Rarely, encephalitis or myelitis or cerebral vasculitis
- CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose
Cardiac Lyme
- AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation
- Resolves with treatment, so only ever needs temporary pacemaker
Late Disease
- Late or chronic (months to years), less inflammatory, usually within a single body site
- Arthritis in 60% of untreated patients, now down to 15-20%
- PCR of synovial fluid
- Encephalomyelitis/encephalopathy next-most common
- LP fairly benign, with slightly elevated protein
- Diagnose with simultaneous serum/CSF antibodies
- Peripheral neuropathy
- Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue
Lyme Arthritis
- Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation
- Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs
Acrodermatitis Chronica Atrophicans
- Chronic red or bluish-red leions, usually on the extensor surgaces
- Initially doughy, eventually atrophic
- Can occur up to 8 years after infection
Late Neuroborreliosis
- Encephalopathy, encephalitis, and peripheral neuropathy
Complications
- Carditis in 5% of untreated patients
- Heart block
- Cardiomyopathy
- Neurologic involvement in 15% of untreated patients
- Uni- or bilateral cranial nerve defects, especially CN VII
- Meningitis and encephalitis
- Migratory arthralgias in 60% of untreated patients
- Conjunctivitis in 10% of untreated patients
- Regional or generalized lymphadenopathy
Borrelial Lymphocytoma
- Painless bluish-red nodule, usually on the ear, nipple, or scrotum
- More common in adults
Ocular Manifestations
- Conjunctivitis, uveitis, papillitis, episcleritis, keratitis
Coinfections
- Anaplasma or Babesia may be transmitted by the same ticks in areas of endemicity
- Can have thrombocytopenia, leukopenia, neutropenia, and anemia
- Hemolytic anemia is highly suggestive of Babesia microti
- Other signs include fever lasting more than one day after start of antibiotics, especially for Babesia microti
Post-Lyme Disease Syndrome
- Subjective symptoms that persist following treatment, without objective clinical findings of infection
Differential Diagnosis
Erythema Migrans
- Tick or insect bite hypersensitivity reaction
- Cellulitis, erysipelas
- Erythema multiforme
- STARI
- Tinea
- Nummular eczema
- Granuloma annulare
- Contact dermatitis
- Urticaria
- Fixed drug eruption
- Pityriasis rosea
- Parvovirus B19 (in children)
Borrelial Lymphocytoma
Lyme Neuroborreliosis
- Other causes of facial nerve palsy
- Viral meningitis
- Mechanical radiculopathy
- First episode of relapsin-remitting multiple sclerosis
- Primary progressive multiple sclerosis
Lyme Carditis
- Other causes of heart block or myopericarditis
Lyme Arthritis
- Gout or pseudogout
- Septic arthritis
- Viral arthritis
- Psoriatic arthritis
- Juvenile oligoarthritis
- Reactive arthritis
- Sarcoidosis
- Early rheumatoid arthritis
- Seronegative spondyloarthropathies
Acrodermatitis Chronic Atrophicans
- Old age
- Chillblains
- Chronic venous insufficiency
- Superficial thrombophlebitis
- Hypostatic eczema
- Arterial obliterative disease
- Acrocyanosis
- Livedo reticularis
- Lymphoedema
- Erythromelalgia
- Scleroderma
- Rheumatoid nodules
- Gouty tophi
- Erythema nodosum
Diagnosis
- Treatment should be based on symptoms and compatible exposure history
- If erythema migrans is present, further testing is unhelpful outside of unusual cases and is not routinely recommended
- The most commonly used test is serology from blood, with EIA followed by reflexive Western blot
- CSF antibodies is useful for neuroborreliosis, but persist years after treatment
- PCR may be helpful in cases where patients are from populations with high seroprevalence
- Pretty good for joint, less sensitive for CSF
Lyme Serology
- Typically done as a screening EIA followed by reflexive Western blot
- In Ontario, the screening test is Borrelia Vls1/pepC10 IgM/IgG ELISA
- The Western blot is done for IgM and IgG
- EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely
- Usually positive around 2 weeks
- False negatives common early in clinical course
- False positives with HIV, hepatitis C, and syphilis
- Cross-reacts with European Lyme
- Western blot split into IgM and IgG if positive or equivocal
- IgM 4 weeks, IgG 8 weeks
- IgM is prone to over-interpretation and false positives
- False positives with spirochetes (syphilis), viruses (cytomegalovirus, Epstein-Barr virus, hepatitis B virus, hepatitis C virus, and parvovirus B19), and bacteria
- Does NOT cross-react with European Lyme (in Ontario)
- Serology is most helpful when the pretest probability is >20%
- Serology remains elevated to months to years and should not be used to monitor response to treatment
| EIA | Western Blot | Interpretation | Action |
|---|---|---|---|
| + | + | Early disseminated or late disease Previous exposure, treated or not |
Treat if compatible symptoms and history |
| + | – | Early disease Early disease, treated European Lyme False-positive |
If <8 weeks from exposure, repeat If >8 weeks, look for other cause Rule out HIV, hepatitis C, and syphilis Assess for autoimmune diseases Consider European Lyme |
| – | – | Very early Lyme <2 weeks Negative |
Treat if erythema migrans |
- Health Canada now recommends a modified two-tier EIA with combined IgM/IgG, with the screening EIA done with whole-cell lysate and the confirmatory EIA done with a recombinant protein
- This approach has increased sensitivity at all stages (50-60% for early Lyme, around 100% for late Lyme including Lyme arthritis), and maintains
- If you get a negative result when there is high pre-test probability for early Lyme, then submit a follow-up serology 3 to 6 weeks later
| EIA 1 | EIA 2 | Interpretation |
|---|---|---|
| – | N/A | Negative; consider alternative diagnosis or resubmit in 3-6 weeks if compatible with early Lyme |
| +/± | +/± | Positive; treat based on clinical syndrome, if appropriate |
| +/± | – | Negative; consider alternative diagnosis or resubmit in 3-6 weeks if compatible with early Lyme |
Management
Erythema Migrans
- Doxycycline 100 mg PO bid for 10 days
- Second-line: amoxicillin 500 mg PO tid for 14 days, cefuroxime 500 mg PO bid for 14 days
- Third-line: azithromycin for 7 days
Neurological Lyme Disease
- Any of the following: ceftriaxone IV, cefotaxime IV, penicillin G IV, doxycycline PO
- Duration of 14 to 21 days
- If there is parenchymal involvement, which is rare and usually based on MRI
- If present, prefer IV antibiotics and a 2 to 4 week course
- In cases of facial nerve palsy, they may also receive corticosteroids within 72 hours
Lyme Carditis
- See Lyme carditis
Lyme Arthritis
- Oral antibiotics for 28 days
- If no response to oral antibiotics, can consider a course of ceftriaxone IV for 2 to 4 weeks
Post-Antibiotic Lyme Arthritis
- Refer to rheumatologist for consideration of DMARDs, biologics, intraarticular steroid injections, or arthroscopic synovectomy
Borrelial Lymphocytoma
- Oral antibiotics for 14 days
Acrodermatitis Chronica Atrophicans
- Oral antibiotics for 21 to 28 days
Prevention
- Routine personal protective measures to reduce tick exposure
- DEET, picaridin, IR3535, oil of lemon eucalyptus, PMD, 2-undecanone, or permethrin
- Remove ticks with clean fine-tipped tweezer inserted between the tick body and the skin
- Do not cover, spray, or burn the tick
- See tick removal for more information
Prophylaxis
- Can be considered in children and adults within 72 hours of tick removal if all of the following criteria are met:
- Ixodes tick is identified
- Small, tear-drop shaped
- Plain oval shield
- Lack of festoons
- Occurs in a highly endemic area
- Tick was attached for ≥36 hours
- You can get a sense by asking if the tick was flat or engorged
- If definitely flat, almost certainly attached less than 36 hours
- However, still looks flat at 24 hours
- Ixodes tick is identified
- Use a single oral dose of doxycycline 4.4 mg/kg (max 200 mg) for children or 200 mg for adults
Further Reading
- 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2020. doi: 10.1093/cid/ciaa1215
- Health Quality Ontario (2018). Management of Tick Bites and Investigation of Early Localized Lyme Disease.