Aminoglycosides
From IDWiki
Background
- Derived from Streptomyces species (mycins & kacins) or Micromonospora species (micins)
Mechanism of Action
- Requires electron transport chain (ETC) to cross over the membrane
- Anaerobes are therefore inherently resistant
- Reversibly binds 30S ribosomal subunit, which stops proofreading and causes accumulation of bad proteins
Spectrum of Activity
- Good coverage of Gram-negative aerobes
- Except Stenotrophomonas and Burkholderia
- Streptomycin also covers mycobacterium
- Some protozoal coverage
- Can cover Gram-positives if cell wall is disrupted (e.g. by beta-lactam)
Mechanisms of Resistance
- Altered 50S ribosomal subunit
- Decreased uptake and accumulation (Pseudomonas)
- Decreased membrane permeability
- Efflux pump (Escherichia coli)
- Aminoglycoside-modifying enzymes (Enterococcus)
Pharmacokinetics and Pharmacodynamics
- Poor membrane penetration, therefore doesn't cross over into lungs and CSF
- Half-life 2-3 hours (longer in CKD)
- Excreted 99% unchanged in urine
- Displays concentration-depedent killing with a prolonged post-antibiotic effect (2-13 hours)
Dosing
Initial Dose
- If actual body weight more than 20% higher than ideal body weight, need to calculate adjusted body weight (ABW)
$$ABW = IBW + 0.4 \times (actual BW - IBW)$$
Traditional Dosing
- Q8H dosing
- Used for Enterococcus IE, meningitis, septic shock, ascites, AKI/CKD, pregnancy, surgical prophylaxis, burns, osteomyelitis
- 1.7mg/kg (5-7.5mg/kg amikacin) IV q8h
Extended Interval Dosing
- Q24H dosing, which is safer but less well-studied
- 7mg/kg (15mg/kg amikacin) IV, frequency depends on CrCl
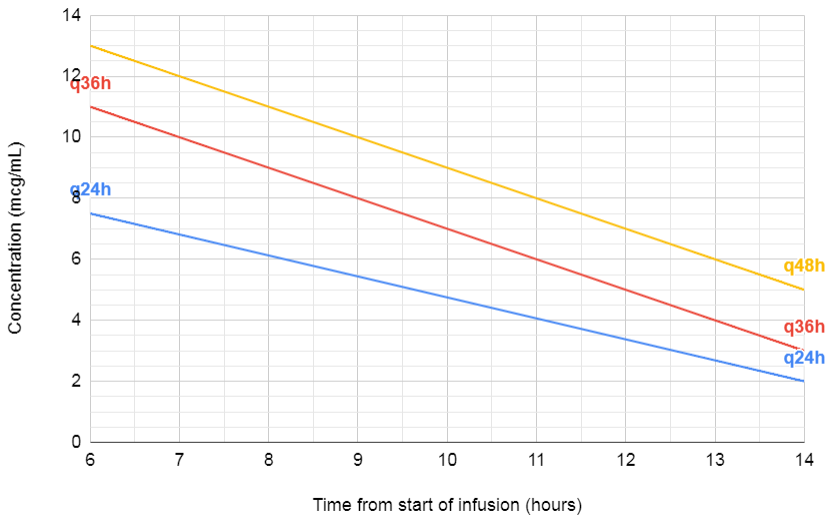
- Use Hartford nomogram with a random level (but remember to halve the amikacin level first)
Dialysis Dosing
- Pre-HD levels with post-HD doses, though this may change
Synergy
- 1mg/kg divided q8-12h, peak target 3-5, trough <2
Monitoring
Peak
- 30 minutes after third dose
- Response is based on peak:MIC ratio, target is 8-10 times
- If below target, increase dose
Trough
- Prior to 4th dose, or a random level at 24 to 48h in renal failure
- Side effects are predicted by trough levels
- Tobramycin <0.5 (extended) or <2 (traditional)
- Amikacin <1 (extended) or <?? (traditional)
- If above target, increase interval
Hartford Nomogram
- Double the concentration for amikacin
Safety
Adverse Drug Reactions
- Nephrotoxicity (0-50%), usually non-oliguric AKI with decreased Ca/Mg resorption, often reversible
- Decreased protein synthesis
- Decreased cellular respiration
- Increased apoptosis
- Necrosis in proximal tubules
- Ototoxicity (0-60%), irreversible
- Cumulative effect
- Distribute into the perilymph of the ear, and cause free radical formation causing apoptosis of hair cells
- Needs hearing tests, because it can be subclinical
- Monitor audiometry weekly
- Vestibulotoxicity (0-20%), irreversible
- Rarely, neuromuscular blockade
Monitoring
- Trough levels
- Creatinine
- Weekly audiometry