Measles virus
From IDWiki
- Highly contagious virus that causes a triad of cough, coryza, and conjunctivitis
Microbiology
- Enveloped RNA Morbillivirus in the Paramyxoviridae family
- Family includes parainfluenza, RSV, measles, mumps
- Eight structural proteins: F, C, H (haemagglutination), L (large), M (matrix), N (nucleoprotein), P (phosphopolymerase), and V
- N, P, and L complex with RNA
- C and V interact with cellular proteins and regulate replication
- M, H, and F are viral envelop proteins
- H helps with host cell attachment, and F helps with spread between cells
Pathophysiology
- Airborne droplets can remain in the air up to 2 hours after a person with measles has coughed
- It is droplet, but just very small droplet
- Innoculated through respiratory mucosa, enters lymphoid cells via SLAM receptor
- SLAM (CDw150) is present on lymphocytes and antigen-presenting cells
- Spreads to entire respiratory systems, as well as intestines, bladder, skin, and spleen, lymph nodes, liver, conjunctiva, and brain
- Propagates within T and B lymphocytes and monocytes, but also endothelial, epithelial, and dendritic cells
- Host response success causes disappearance of serology and appearance of rash
- Possibly the rash represents a hypersensitivity reaction to the virus mediated by cellular immunity
Epidemiology
- Infection confers lifelong immunity, though vaccination may not
- Worldwide distribution
- Prior to vaccination, there were epidemics every 2 to 5 years lasting 3 to 4 months
- Vaccine hesitancy is becoming more common
- Parts of Europe
Differential Diagnosis
- Rubella
- Kawasaki syndrome
- Scarlet fever
- Roseola
- Infectious mononucleosis
- Risckettsial infections
- Enteroviral infections
- Adenoviral infections
Clinical Presentation
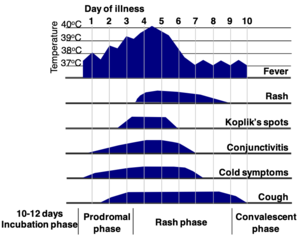
- Incubation period 10-14 days (range up to 21 days), followed by several days of prodrome that includes fever, anorexia, cough, coryza, and conjunctivitis
- Can be mistaken for common cold or for Kawasaki disease
- Koplik spots appear at end of prodrome
- Bluish gray specks on a red base in the oral mucosa ("like grains of sand")
- Rash follows Koplik spots
- Spreads from face to body, including palms and soles
- Fevers resolve soon after rash appears
- Rash is erythematous and maculopapular, and my desquamate as it begins to heal
- Usually lasts 5 days, clearing in the same pattern that it appeared
- The rash disappears about 7 to 10 days after late prodromal period, with cough being the last symptom to disappear
Complications
- Respiratory involvement, either as primary infection of with bacterial superinfection
- Otitis media, pneumonia (on CXR, even if uncomplicated)
- Acute encephalitis, which can have sequelae
- Blindness, corneal scarring
- Hepatitis
- Complications are more common in adults who are infected
Subacute sclerosing panencephalitis (SSPE)
- Degenerative neurological condition caused by persistent CNS infection despite immune response
- 5-10 years after infection
- Higher risk if infection before age 2 years
- Inevitably ends in death
Special Populations
Modified measles
- Patients with passive immunity to measles may present with a milder form
- Babies with mom's immunoglobulin, or patients who have received immune globulin
- The prodrome, Koplik spots, and rash are often absent, and it is sometimes subclinical
Atypical measles
- Patients with prior immunization with killed vaccine (no longer on market, since 1960s) may have an atypical presentation
- Prodrome of fever and pain for 1 to 2 days
- Rash follows, but moves peripherally to centrally, and have varied form (urticarial, maculopapular, hemorrhagic, vesicular)
- Can mimic vaicella, RMSF, HSP, drug eruption, or toxic shock syndrome
- Fever continues, with edema, interstitial pneumonia, hepatitis, and occasionally pleural effusion
- More prolonged course, with very high antibody titres
Immunocompromised
- Chemotherapy, transplantation, AIDS, and congenital cellular immunodefieciency are all risk factors for severe measles
- Possibly also malnutrition
- Can develop giant cell pneumonia, without rash, as well as a chronic encephalitis
- Can detect measles RNA in brain tissue
Pregnancy
- Can be severe
- Can cause spontaneous abortion and premature delivery
- Newborn can be infected; they should get immune globulin at birth
Diagnosis
- Typically diagnosed clinically; CBC may show leukopenia
- If uncertain of the diagnosis, can use serology or molecular tests to confirm
- NP swab PCR within 7 days of rash onset
- Urine PCR within 14 days of rash onset
- ELISA IgG serology, repeated after 1 week; fourfold titre increase is diagnostic
- Or IgM, if available, to diagnose on one sample
- IgM can persist for up to a month
- Viral culture is also possible
- For SSPE, can demonstrate high titres in serum and CSF
Management
- Most infectious just before rash; quickly becomes non-infectious after end of prodrome
- Supportive care
- Vitamin A can be given, especially if the child is deficien
- In children >1 year, vitamin A 200,000 IU daily for 2 days
- If 6-12 months old, use 100,000 IU for 2 days
- Less than 6 months, use 50,000 IU
- If deficient, give another dose at 2 to 4 weeks
- Ribavirin unhelpful but sometimes given
Infection control
- Infectious period is 5 days prior to rash and 4 days after, in general, though infectiousness starts with respiratory involvement
- Need to do contact tracing, including people up to two hours after any room they were in
- All contacts should be quarantined at home regardless of symptoms
Post-exposure prophylaxis (PEP)
- Indications for passive immunization with immune globulin
- High risk for severe or fatal measles and are susceptible
- Includes children with malignancy, cell-mediated immunodeficiency (including AIDS), and possibly babies <1 year
- Must be given within 6 days of exposure
- Infants <1 year: IMIg 0.25 mL/kg once
- Other children: IMIg 0.5 mL/kg once (maximum of 15 mL)
- Immunization for post-exposure prophylaxis can be done in other, immunocompetent patients
- Can shorten the time to rash, suggesting a shorter period of infectiousness
Vaccination
- Live vaccine given in MMR at 12-15 months, with a booster later in childhood
- Don't vaccinate for 5-6 months after receiving immune globulin
- No adverse effects of revaccination
- Rates need to be >95% to prevent imported cases from causing outbreaks
- Rates less than 80% allow endemic transmission with cyclical outbreaks every 3-5 years
- Vaccination is contraindicated in AIDS, other cell-mediated immunodeficiency, and in pregnancy
- Wait 3 months after chemotherapy
- Don't use MMRV, since no safety data are available
- Can be associated with anaphylaxis in patients with true egg allergy
Vaccine failure
- Improper storage >4º C
- Failure to use proper diluent for lyophilized vaccine
- Exposure to light or heat
- Vaccination in the presence of passive antibody