Borrelia burgdorferi: Difference between revisions
From IDWiki
Borrelia burgdorferi
Content deleted Content added
No edit summary |
|||
| Line 1: | Line 1: | ||
= Epidemiology = |
== Epidemiology == |
||
== North America == |
=== North America === |
||
* Transmitted by ''[[Ixodes scapularis]]'' (deer or black-legged tick), or ''[[I. pacificus]]'' in the Pacific US |
* Transmitted by ''[[Ixodes scapularis]]'' (deer or black-legged tick), or ''[[I. pacificus]]'' in the Pacific US |
||
| Line 11: | Line 11: | ||
[[File:image-20190117091839996.png|image-20190117091839996]] |
[[File:image-20190117091839996.png|image-20190117091839996]] |
||
== Europe == |
=== Europe === |
||
* Three species of ''[[Borrelia]]'' exist in Europe |
* Three species of ''[[Borrelia]]'' exist in Europe |
||
| Line 19: | Line 19: | ||
* The species have cross-reactivity with Lyme serology |
* The species have cross-reactivity with Lyme serology |
||
= Life Cycle = |
== Life Cycle == |
||
[[File:lifecycle.jpg|tick lifecycle]] |
[[File:lifecycle.jpg|tick lifecycle]] |
||
= Pathophysiology = |
== Pathophysiology == |
||
* Tick bites host |
* Tick bites host |
||
| Line 29: | Line 29: | ||
* Local multiplication followed by dissemination |
* Local multiplication followed by dissemination |
||
= Risk Factors = |
== Risk Factors == |
||
* Hiking or camping in Vermont or other endemic area, with known or possible tick exposure |
* Hiking or camping in Vermont or other endemic area, with known or possible tick exposure |
||
= Clinical Presentation = |
== Clinical Presentation == |
||
* May not remember tick bite |
* May not remember tick bite |
||
* There can be overlap between the three stages (early localized, early disseminated, late) |
* There can be overlap between the three stages (early localized, early disseminated, late) |
||
== Early localized disease (7 days) == |
=== Early localized disease (7 days) === |
||
* Presents within 1 month of exposure |
* Presents within 1 month of exposure |
||
| Line 50: | Line 50: | ||
* May have mildly elevated liver enzymes |
* May have mildly elevated liver enzymes |
||
== Early disseminated disease (14-21 days) == |
=== Early disseminated disease (14-21 days) === |
||
* Early disseminated (weeks to months), inflammatory phase |
* Early disseminated (weeks to months), inflammatory phase |
||
| Line 58: | Line 58: | ||
* Cranial nerve palsies, lymphocytic meningitis, conjunctivitis, arthralgia, myalgia, headache, fatigue, carditis (heart block) |
* Cranial nerve palsies, lymphocytic meningitis, conjunctivitis, arthralgia, myalgia, headache, fatigue, carditis (heart block) |
||
== Neuroborreliosis == |
=== Neuroborreliosis === |
||
* Meningo-radiculitis, meningitis, and peripheral facial palsy |
* Meningo-radiculitis, meningitis, and peripheral facial palsy |
||
* CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
* CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose |
||
== Cardiac Lyme == |
=== Cardiac Lyme === |
||
* AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation |
* AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation |
||
* Resolves with treatment, so only ever needs temporary pacemaker |
* Resolves with treatment, so only ever needs temporary pacemaker |
||
== Late disease == |
=== Late disease === |
||
* Late or chronic (months to years), less inflammatory, usually within a single body site |
* Late or chronic (months to years), less inflammatory, usually within a single body site |
||
| Line 79: | Line 79: | ||
* Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue |
* Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue |
||
== Lyme arthritis == |
=== Lyme arthritis === |
||
* Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation |
* Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation |
||
* Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs |
* Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs |
||
== Acrodermatitis chronica artophicans == |
=== Acrodermatitis chronica artophicans === |
||
* Chronic red or bluish-red leions, usually on the extensor surgaces |
* Chronic red or bluish-red leions, usually on the extensor surgaces |
||
| Line 90: | Line 90: | ||
* Can occur up to 8 years after infection |
* Can occur up to 8 years after infection |
||
== Late neuroborereliosis == |
=== Late neuroborereliosis === |
||
* Encephalopathy, encephalitis, and peripheral neuropathy |
* Encephalopathy, encephalitis, and peripheral neuropathy |
||
== Complications == |
=== Complications === |
||
* Carditis in 5% of untreated patients |
* Carditis in 5% of untreated patients |
||
| Line 106: | Line 106: | ||
* Regional or generalized lymphadenopathy |
* Regional or generalized lymphadenopathy |
||
== Borrelial lymphocytoma == |
=== Borrelial lymphocytoma === |
||
* Painless bluish-red nodule, usually on the ear, nipple, or scrotum |
* Painless bluish-red nodule, usually on the ear, nipple, or scrotum |
||
* More common in adults |
* More common in adults |
||
== Ocular manifestations == |
=== Ocular manifestations === |
||
* Conjunctivitis, uveitis, papillitis, episcleritis, keratitis |
* Conjunctivitis, uveitis, papillitis, episcleritis, keratitis |
||
== Coinfection == |
=== Coinfection === |
||
* Can have thrombocytopenia and anemia if coinfected with ''Anaplasma'' or ''Babesia'' |
* Can have thrombocytopenia and anemia if coinfected with ''Anaplasma'' or ''Babesia'' |
||
== Post-Lyme disease syndrome == |
=== Post-Lyme disease syndrome === |
||
* Subjective symptoms that persist following treatment, without objective clinical findings of infection |
* Subjective symptoms that persist following treatment, without objective clinical findings of infection |
||
= Diagnosis = |
== Diagnosis == |
||
* Treatment should be based on symptoms and compatible exposure history |
* Treatment should be based on symptoms and compatible exposure history |
||
| Line 142: | Line 142: | ||
** Pretty good for joint, less sensitive for CSF |
** Pretty good for joint, less sensitive for CSF |
||
== Lyme Serology == |
=== Lyme Serology === |
||
{| |
{| |
||
| Line 166: | Line 166: | ||
|} |
|} |
||
= Management = |
== Management == |
||
* Doxycycline 100mg po BID x14 days |
* [[Doxycycline]] 100mg po BID x14 days |
||
** 7 to 21 days, depending on severity |
** 7 to 21 days, depending on severity |
||
* Alternative: amoxicillin 500mg po TID or cefuroxime 500mg po BID or azithromycin |
* Alternative: [[amoxicillin]] 500mg po TID or [[cefuroxime]] 500mg po BID or [[azithromycin]] |
||
* Parenteral antibiotics for CNS or cardiac disease |
* Parenteral antibiotics for CNS or cardiac disease |
||
= Further Reading = |
== Further Reading == |
||
* Health Quality Ontario (2018). [https://www.hqontario.ca/Evidence-to-Improve-Care/Evidence-and-Health-Quality-Ontario/Guidance-Documents Management of Tick Bites and Investigation of Early Localized Lyme Disease]. |
* Health Quality Ontario (2018). [https://www.hqontario.ca/Evidence-to-Improve-Care/Evidence-and-Health-Quality-Ontario/Guidance-Documents Management of Tick Bites and Investigation of Early Localized Lyme Disease]. |
||
Revision as of 20:07, 15 August 2019
Epidemiology
North America
- Transmitted by Ixodes scapularis (deer or black-legged tick), or I. pacificus in the Pacific US
- Reservoirs include deer and small mammals such as rodents
- Lyme species are different outside of North America

Europe
- Three species of Borrelia exist in Europe
- B. burgdorferi
- B. afzelii
- B. garinii
- The species have cross-reactivity with Lyme serology
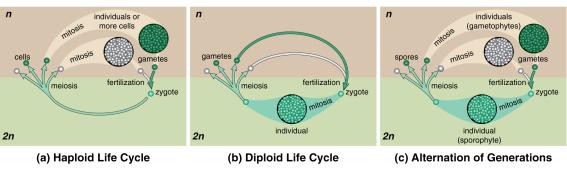
Life Cycle
Pathophysiology
- Tick bites host
- Borrelia migrates from hidgut to mouth over ~36 hours, then gets regurgitated into the wound
- Local multiplication followed by dissemination
Risk Factors
- Hiking or camping in Vermont or other endemic area, with known or possible tick exposure
Clinical Presentation
- May not remember tick bite
- There can be overlap between the three stages (early localized, early disseminated, late)
Early localized disease (7 days)
- Presents within 1 month of exposure
- Erythema migrans in 80%; appears 7-14 days after tick bite (range 3 to 32 days)
- If appears immediately and rapidly, think about local irritation and allergy, rather than Lyme
- Can present atypically, without target appearance, with ulceration, or with vesicles
- Spreads 2-3 days daily
- Fever, fatigue, malaise, lethargy
- Mild headache and neck stiffness
- Myalgias and arthralgias
- May have mildly elevated liver enzymes
Early disseminated disease (14-21 days)
- Early disseminated (weeks to months), inflammatory phase
- Non-specific febrile illness
- Bell palsy, aseptic meningitis, and heart block
- Multiple rashes
- Cranial nerve palsies, lymphocytic meningitis, conjunctivitis, arthralgia, myalgia, headache, fatigue, carditis (heart block)
Neuroborreliosis
- Meningo-radiculitis, meningitis, and peripheral facial palsy
- CSF shows lymphocytic pleocytosis, slightly elevated protein, and normal glucose
Cardiac Lyme
- AV conduction dysfunction, arrhythmia, and sometimes myocarditis or pericarditis, without other explanation
- Resolves with treatment, so only ever needs temporary pacemaker
Late disease
- Late or chronic (months to years), less inflammatory, usually within a single body site
- Arthritis in 60% of untreated patients, now down to 15-20%
- PCR of synovial fluid
- Encephalomyelitis/encephalopathy next-most common
- LP fairly benign, with slightly elevated protein
- Diagnose with simultaneous serum/CSF antibodies
- Peripheral neuropathy
- Affects heart, nervous system and joints; arrhythmias, heart block and sometimes myopericarditis; recurrent arthritis affecting large joints (i.e., knees); peripheral neuropathy; central nervous system manifestations – meningitis; encephalopathy (i.e., behavior changes, sleep disturbance, headaches); and fatigue
Lyme arthritis
- Recurrent attacks or persisting arthritis involving one or more large joints, without other explanation
- Arthrocentesis shows 25,000 cells (range 500 to 110,000), mostly PMNs
Acrodermatitis chronica artophicans
- Chronic red or bluish-red leions, usually on the extensor surgaces
- Initially doughy, eventually atrophic
- Can occur up to 8 years after infection
Late neuroborereliosis
- Encephalopathy, encephalitis, and peripheral neuropathy
Complications
- Carditis in 5% of untreated patients
- Heart block
- Cardiomyopathy
- Neurologic involvement in 15% of untreated patients
- Uni- or bilateral cranial nerve defects, especially CN VII
- Meningitis and encephalitis
- Migratory arthralgias in 60% of untreated patients
- Conjunctivitis in 10% of untreated patients
- Regional or generalized lymphadenopathy
Borrelial lymphocytoma
- Painless bluish-red nodule, usually on the ear, nipple, or scrotum
- More common in adults
Ocular manifestations
- Conjunctivitis, uveitis, papillitis, episcleritis, keratitis
Coinfection
- Can have thrombocytopenia and anemia if coinfected with Anaplasma or Babesia
Post-Lyme disease syndrome
- Subjective symptoms that persist following treatment, without objective clinical findings of infection
Diagnosis
- Treatment should be based on symptoms and compatible exposure history
- If EM present, further testing is unhelpful outside of unusual cases
- Usually done by serology, with EIA followed by reflexive Western blot
- EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely
- Usually positive around 2 weeks
- False negatives common early in clinical course
- False positives with HIV, hepatitis C, and syphilis
- Cross-reacts with European Lyme
- Western blot split into IgM and IgG if positive or equivocal
- IgM 4 weeks, IgG 8 weeks
- IgM is prone to over-interpretation and false positives
- Does NOT cross-react with European Lyme (in Ontario)
- Serology is most helpful when the pretest probability is >20%
- EIA should be positive by 4 to 6 weeks; if negative, Lyme is unlikely
- CSF antibodies is useful for neuroborreliosis, but persist years after treatment
- PCR may be helpful in cases where patients are from populations with high seroprevalence
- Pretty good for joint, less sensitive for CSF
Lyme Serology
| EIA | Western blot | Interpretation | Action |
|---|---|---|---|
| + | + | Early disseminated or late disease Previous exposure, treated or not |
Treat if compatible symptoms and history |
| + | – | Early disease Early disease, treated European Lyme False-positive |
If <8 weeks from exposure, repeat If >8 weeks, look for other cause Rule out HIV, hepatitis C, and syphilis Assess for autoimmune diseases Consider European Lyme |
| – | – | Very early Lyme <2 weeks Negative |
Treat if erythema migrans |
Management
- Doxycycline 100mg po BID x14 days
- 7 to 21 days, depending on severity
- Alternative: amoxicillin 500mg po TID or cefuroxime 500mg po BID or azithromycin
- Parenteral antibiotics for CNS or cardiac disease
Further Reading
- Health Quality Ontario (2018). Management of Tick Bites and Investigation of Early Localized Lyme Disease.