Background
Microbiology
- Cestode (tapeworm)
- Scolex (head) attached to strobila (body), which is composed of proglottids
- Each proglottid contains male and female sexual organs
- Each proglottid fills itself with eggs, then detaches, breaking down and releasing eggs
- The proglottids are not motile, unlike T. saginata
- Can grow up to 2 to 8 m in length
Life Cycle
- Definitive host (e.g. humans) ingests meat (usually undercooked pork) containing viable cysts
- The cysts develop into the tapeworms, releasing embryonated eggs into the environment
- The tapeworms can live for 10 to 20 years
- Intermediate host (e.g. humans or pigs) ingests eggs in fecally-contaminated food
- The egg invades into the organism, disseminates hematogenously, and forms a cyst in tissue
- Unique to T. solium is that humans can be both definitive and intermediate hosts
- The human can become infected by autoinnoculation
Pathophysiology
- The adult tapeworms are very well tolerated, though they can decrease gut absorption
Epidemiology
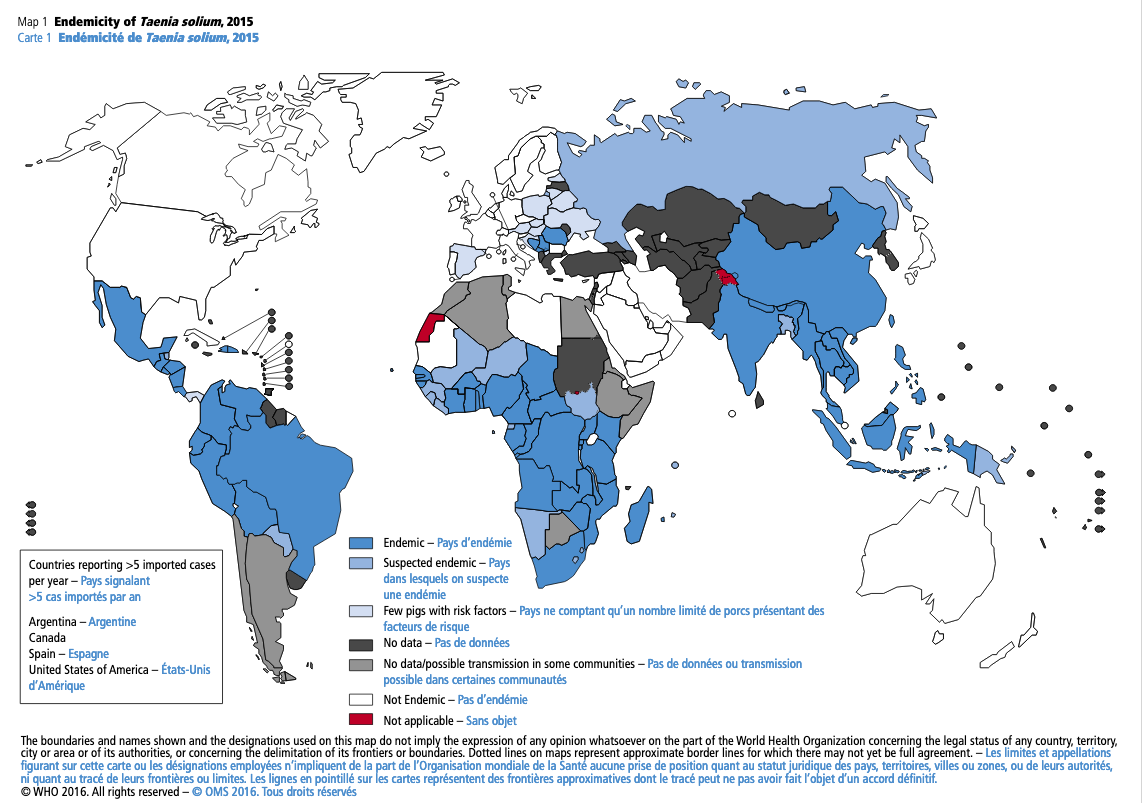
- Common in Mexico, Central America, South America, the Philippines, and Southeast Asia
- ~20-25% of randomly-selected people with have calcifications or serology consistent
- Neurocysticercosis causes ~50,000 deaths annually worldwide
- Also one of the leading causes of seizure worldwide
- Usually acquired abroad, but there are cases of local acquisition from within the household
- Risk factors for cysticercosis include:
- Residence in endemic country
- Increasing age
- Frequent consumption of pork
- Poor household hygiene
Clinical Presentation
- Can be infected with the tapeworm (i.e. as definitive host) or with the cysts (i.e. as intermediate host), or with both (~25% of infections)
Taeniasis
- No specific symptoms, though may cause some element of malnutrition
- Can become symptomatic if autoinnoculation occurs
Cysticercosis
- Cysts can go anywhere, with the most dangerous and symptomatic locations being the heart and the brain
- They will eventually die and calcify, but will still be seen on plain X-ray
Neurocysticercosis
- Incubation period is usually 3 to 5 years but can be up to 30 years
- Most commonly presents with seizure (70%) or intracranial hypertension
- Intraparenchymal cerebral cysts enlarge slowly, asymptomatic for years or decades until they begin to die, causing inflammation
- They can leak, provoking inflammation with cerebritis and meningitis
- These can lead to focal or generalized seizures, focal neurological deficits, intellectual impairment, psychiatric disorders, and hydrocephalus
- Intraventricular and basilar cysts present earlier
- Obstruction of CSF or local meningeal irritation
- Can cause cranial nerve or brainstem deficits
- Racemose cysticercosis (aggressive basilar neurocysticercosis) occurs when cysts proliferate at the base of the brain, causing coma and death
- Cysticercotic encephalitis occurs when there is a massive infection of the brain parenchyma
- Intraparenchymal spinal cord lesions can become symptomatic early due to local effects, or more slowly if outside the cord itself
- Ophthalmologic cysticercosis
Cardiac cysticercosis
- Rare, but can cause heart failure and conduction abnormalities
Diagnosis
Taeniasis
- Stool O&P
- Eggs are indistinguishable from T. saginata, so ideally needs a proglottid for diagnosis
- If seen, consider looking for concommitant cysts
Cysticercosis
- No single diagnostic test, but rather a combination of epidemiology, clinical presentation, imaging, and supportive laboratory investigations
- CSF for neurocysticercosis shows lymphocytic or eosinophilic pleiocytosis, hypoglycorrhachia, and elevated protein
- Can send lentil lectin glycoprotein Western blot (LLGP-WB) or antibody testing, but sensitivity is proportional to number of lesions
- Serology is available, with enzyme-linked immunotransfer blot
- Sensitivity high, but only confirms previous exposure
- Sensitivity low in cases of only one cyst
- High turnaround time
Neuroimaging
- Imaging with both non-contrast CT and MRI
- Shows multiple enhancing and nonenhancing unilocular cysts
- Average of 7 to 10 per patient
- Appearance on MRI depends on stage of development
- Vesicular cysticerci are small and rounded, without edema, and can have a pathognomonic eccentric hyperdense nodule (represents the scolex)
- Early vesicular stage shows smooth, thin-walled cysts, rarely with edema and contrast enhancement, but with a scolex often present
- Typically <2 cm in diameter
- The mural nodule of the scolex is pathognomonic
- In the colloidal-vesicular stage, as the cyst degenerates, pericystic edema and cyst wall enhancement are visible
- In the granular nodular stage, edema and contrast enhancement persist, with the cyst isointense on T1 and iso- to hypointense on T2
- In the quiescent or residual stage, only small calcified nodules without mass effect and usually without enhancement are seen
- Colloidal and granular cysticerci are il-defined, with surrounding edema
- Calcified cysts can be detected on CT as hyperdense nodules without contrast enhancement
Classification of Neurocysticercosis
| Form | Imaging | Histopathology |
|---|---|---|
| Parenchymal | ||
| Non-viable, calcified | Nodular calcifications <20 mm in diameter with or without edema and/or contrast enhancement | Calcified granuloma with or without surrounding inflammation and/or gliosis |
| Single, small enhancing | Cystic or nodular enhancing lesion <2 cm in size | Single parenchymal parasite in the process of degeneration with surrounding inflammation and variable opacification or absence of the cyst fluid |
| Viable parenchymal | Vesicular lesions often with evidence of associated contrast enhancement and/or surrounding edema; scolex often visible on high-definition | Parasites with intact cyst wall, vesicular fluid and scolex, with variable inflammation suurounding the parasite sometimes invading cyst wall |
| Extraparenchymal | ||
| Intraventricular | Cysticerci within the ventricles, obstructive hydrocephalus or loculated hydrocephalus with disproportionate dilatation of the ventricles | Viable cysticercus cyst within the ventricle and/or obstructive hydrocephalus |
| Subarachnoid | Cysticerci in the Sylvian fissure, in the basilar cisterns, or interhemispheric spaces. Strokes or meningitis without discrete cysts. | Cysticerci in the subarach space with arachnoiditis and vasculitis. The cysticerci are often in clusters with proliferating memranges (racemose) and may lack scolex |
| Spinal | Cysticerci within spinal subarach space with or without inflammation/arachnoiditis. Intramedullary cysticerci within the spinal cord | Subarach cysticerci often with associated arachnoiditis. Intramedullary csticerci similar pathologically to parenchymal cysticerci |
Diagnostic Criteria
- Parenchymal neurocysticercosis
- Definitive parenchymal neurocysticercosis, one of the following:
- Parenchymal cyst with pathological diagnosis
- Single or multiple active parenchymal cysts, with at least one cyst with scolex on CT or MRI
- Multiple parenchymal vesicles without scolex associated with at least one of the following:
- Seizures: focal or generalized tonic‐clonic
- Positive serum or CSF immunological test (ELISA, EITB)
- Any combination of the parenchymal cysticercus in different evolutive stages: vesicular with or without scolex, degenerative (colloidal or nodular), and calcified
- Probable parenchymal neurocysticercosis, one of the following:
- Single parenchymal calcification or vesicle (without scolex) or degenerating cyst(s), establishing differential diagnoses with other etiologies, associated with at least two of the following:
- Seizures: focal or generalized tonic‐clonic
- Subcutaneous or muscle cysts location confirmed by biopsy
- Positive serum or CSF immunological test (ELISA, EITB)
- Plain X‐ray films showing “cigar‐shaped” calcifications
- Individual who lives or has lived in or has traveled frequently to endemic countries
- Multiple parenchymal calcifications in an individual who lives or has lived in or has traveled frequently to endemic countries and in whom clinical state excludes other etiologies of calcifications
- Single parenchymal calcification or vesicle (without scolex) or degenerating cyst(s), establishing differential diagnoses with other etiologies, associated with at least two of the following:
- Definitive parenchymal neurocysticercosis, one of the following:
- Extraparenchymal neurocysticercosis (intraventricular/basal subarachnoid)
- Definitive extraparenchymal neurocysticercosis, one of the following:
- Extraparenchymal cyst with pathological diagnosis
- One or more extraparenchymal cysts on MRI special sequences with scolex in at least one of them
- One or more extraparenchymal cysts on MRI special sequences without scolex associated with at least two of the following:
- Hydrocephalus
- Inflammatory CSF
- Positive CSF immunological test (ELISA, EITB)
- Presence of single or multiple calcifications or parenchymal vesicular or degenerative cyst
- Definitive extraparenchymal neurocysticercosis, one of the following:
- Definitive parenchymal and extraparenchymal neurocysticercosis
- Combination of the above definitive parenchymal and definitive extraparenchymal criteria
Management
Adult Tapeworm
- Praziquantel 5 to 10 mg/kg once
- Well-tolerated, cysticidal
- Niclosamide 2 g once
- Not absorbed, stays in the gut, therefore only kills the adult worms
- Don't treat during pregnancy unless necessary
Cysticercosis
- Surgical resection and antihelminthic therapy both can be used
- Screen everyone for ophthalmologic cysticercosis before treatment
Neurocysticercosis
- Non-contrast CT (for calcifications) and MRI brain
- Screen for LTBI if likely to need long steroids
- Screen for Strongyloides if likely to need long steroids
- Fundoscopy prior to starting antihelminthic
- Screen household members
Intraparenchymal Lesions
- Indications
- Treat if viable cysts
- Don't treat if only calcified cysts
- May not need treatment if they are from India (overall good prognosis)
- Antiparasitic
- If 1-2 viable cysticerci: albendazole 15 mg/kg/day (max 1200 mg/day) divided bid for 10 to 14 days with food
- 60% resolve spontaneously by 1-2 years
- Medications may increase time to resolution, but will lower risk of seizure recurrence
- If >2 viable cysticerci: albendazole 15 mg/kg/day plus praziquantel 50 mg/kg/day for 10 to 14 days
- If only calcified cysticerci: supportive treatment only
- If diffuse encephalitis: avoid treating
- If 1-2 viable cysticerci: albendazole 15 mg/kg/day (max 1200 mg/day) divided bid for 10 to 14 days with food
- Adjuncts
- Adjunctive corticosteroids for all for 6-8 weeks then taper
- Need to start at least 24 hours before starting antiparasitic
- If refractory seizures, consider neurosurgery service
- Antiepileptic medications, which may later be tapered
- Adjunctive corticosteroids for all for 6-8 weeks then taper
- Monitoring
- Monitor liver enzymes and leukopenia if >14+ days
- MRI every 6 months until resolution
- Re-treat if parenchymal cysts persist for 6 months after initial treatment
Extraparenchymal and Intraventricular Lesions
- Neurosurgical removal with minimally-invasive neuroendoscopy for lateral and third ventricles, and possibly fourth ventricle
- If unable to, may need VP shunt
- Corticosteroids perioperatively
- Antihelminthic therapy only necessary in those that cannot have surgical removal
Subarachnoid Lesions
- Screen with spinal MRI for concommitant spinal cysticercus
- Treat with antihelminthic until radiographic resolution on MRI (at least 2-3 months, can be more than a year)
- Variable response with high rate of relapse
- Corticosteroids prior to antiparasitic drugs
- Consider methotrexate as steroid-sparing agent
- VP shunt preferred to neurosurgery
Spinal Lesions
- Consider steroids and antihelminthic, as well as surgical options
Ocular Lesions
- Surgical removal
Pregnancy
- Defer antihelminthic until after pregnancy, if possible
Prevention
- Mainly prevented by good sanitation, animal husbandry, and food preparation
- Cook meats thoroughly, or freeze them thoroughly
Further Reading
- Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the IDSA and ASTMH. Clin Infect Dis. 2018;66(8):e49-e75.
- New diagnostic criteria for neurocysticercosis: Reliability and validity. Ann Neurol. 2016;80(3):434-442.